Strokes are the fifth leading cause of death in the United States and a major cause of long-term disability. Thankfully, great strides have been made in treating patients who have had strokes and been left with a disability. Ekso Bionics is leading the way with robotic exoskeletons to help those who have lost mobility due to stroke, spinal cord injury, or brain injury regain what they have lost.
What Is a Stroke?
A stroke occurs when part of the brain is deprived of oxygen. This can be caused by a blood clot blocking blood flow or by a rupture in the artery feeding blood to that part of the brain. Either way, if blood flow is not returned to the affected part of the brain quickly, the damage to the brain can become permanent. This can result in varying degrees of disability or death.
There is also a type of stroke that is temporary. Known as a transient ischemic attack (TIA), these happen when the blood supply to the brain is cut off for only a short time. After experiencing a TIA, a patient may become clumsy or confused, but the effects are only temporary. Once blood flow returns to the brain, the effects of the TIA dissipate. It is still vital to see a doctor after having a TIA. People who frequently have these attacks may have a full-blown stroke later on.
Immediate treatment can sometimes reverse the effects of a stroke. In the case of permanent stroke damage, rehabilitation with EksoNR exoskeleton can successfully return patients to a lifestyle similar to the one they enjoyed previously. You can read more about the research on EksoNR and stroke in our Clinical Summary. This transformative device has been helping adults of all ages regain their mobility and their quality of life.
Health Effects of a Stroke
Because the brain controls almost all of our bodily functions, the range of effects from a stroke is very broad. Frequently, patients who have had a stroke have complete or partial paralysis to one side of their body, including the facial muscles. This can manifest as drooping eyelids, an inability to speak or chew food properly, and reduced mobility.
Sometimes strokes do not affect a person’s limbs and muscles but rather the parts of the brain that control thinking, speech, hearing, or eyesight. In these cases, a patient may have a diminished ability to think clearly or logically. They may show personality changes or lose their memory. If the areas of the brain that control the senses are damaged, the result may be loss of taste, smell, hearing, or sight.
Even with advances in understanding strokes, it is still somewhat unpredictable how a stroke will affect someone. If the patient’s symptoms include decreased mobility, even if it is severe, EksoNR robotic exoskeleton can be a powerful tool for reversing this potentially life altering side effect.
Stroke Treatments
Stroke treatments fit into two categories: preventative treatments and rehabilitative treatments to regain what was lost.
Preventative Stroke Treatments
Immediate stroke treatments vary depending on how the stroke occurred. If a blood clot caused the stroke, then medications will be given to thin the blood and reduce the size of the clot. If a rupture or other brain bleed caused the stroke, steps would be taken to stop the bleeding and return blood flow to that part of the brain.
In both instances, medication is often given to reduce the patient’s blood pressure. High blood pressure can be both a cause and a result of a stroke.
Rehabilitative Stroke Treatments
Rehabilitative stroke treatments begin after any chance of reversing the damage through medical means has passed. These treatments are designed to strengthen weakened muscles, reteach parts of the brain to take over for the damaged areas, and help the patient adapt to a new way of doing things. While physical, speech, and occupational therapy is a part of these treatments, new technology, like EksoNR, gives patients who have had a stroke that resulted in paralysis or loss of mobility more options, and hope.
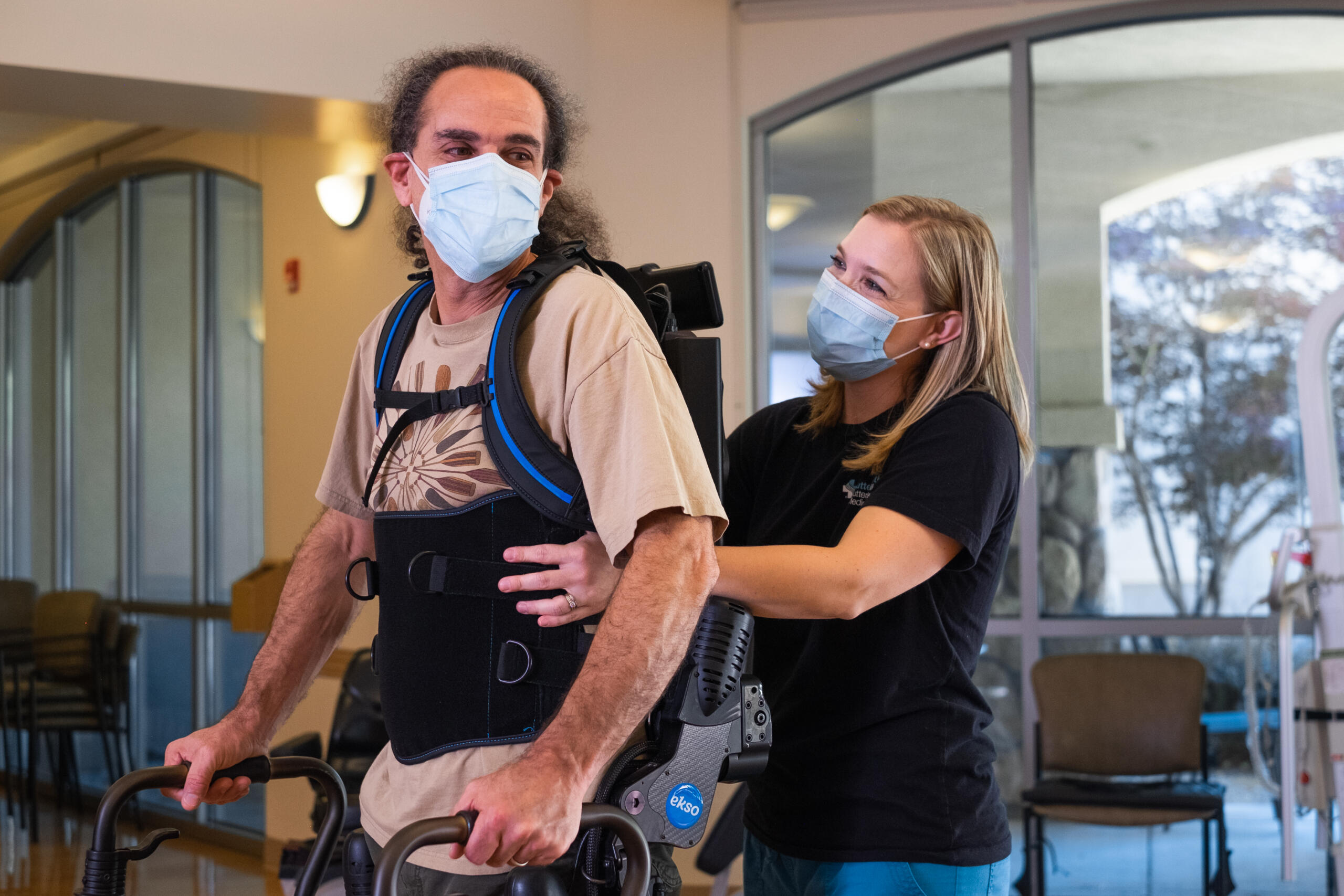
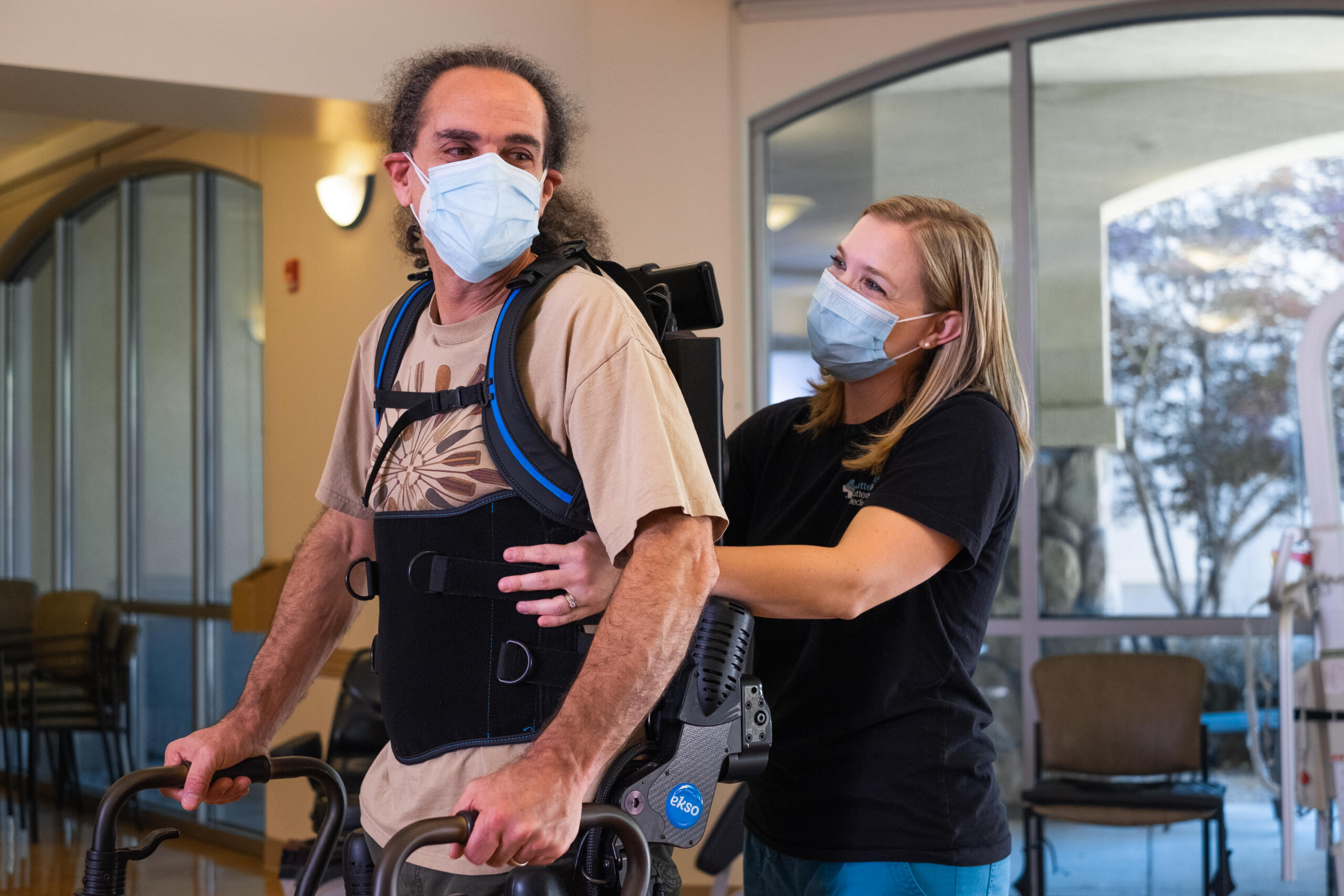
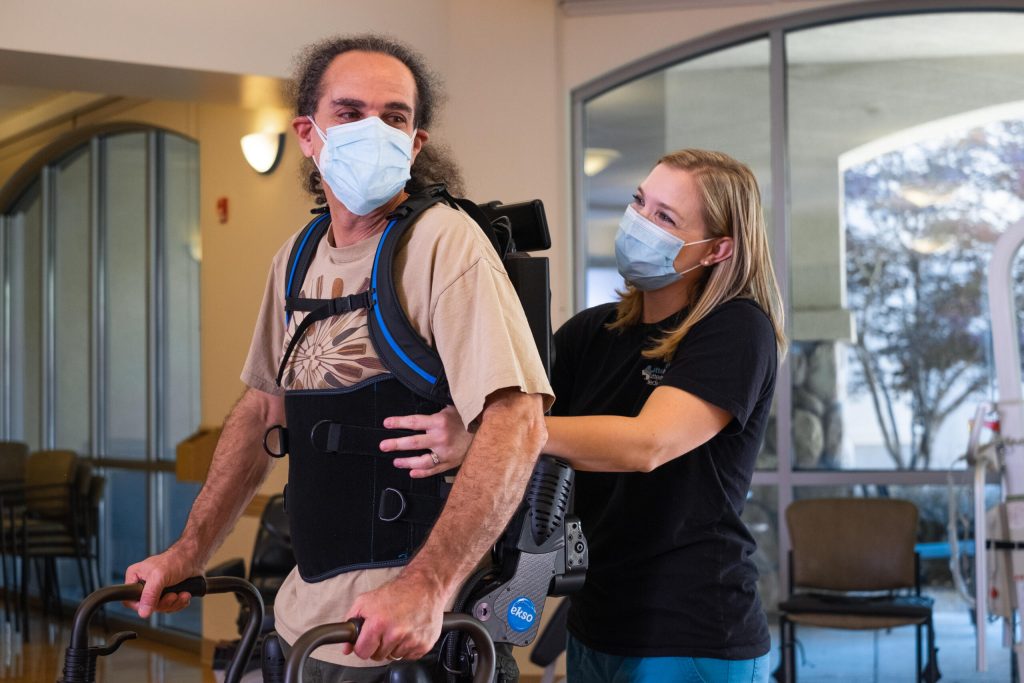
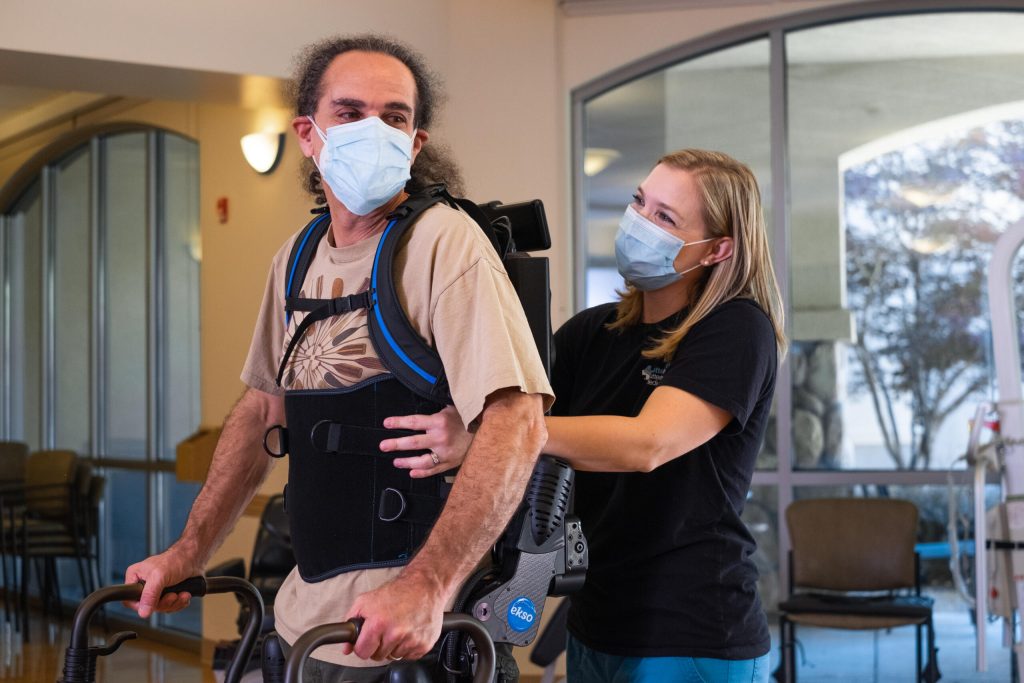
EksoNR is a robotic exoskeleton that the Food and Drug Administration has cleared for rehabilitation after stroke. It provides therapists the opportunity to work with patients’ brain plasticity and retrain their muscles and brains to regain lost mobility. It has shown great success at helping thousands of patients leave their wheelchairs or walkers behind.
EksoNR can be utilized both in walking and preGait modes. Pre-gait activities include those that work on balance, midline orientation, and prepare a patient for walking.
The various gait-training modes offer support to the torso, hips, knees, and ankles while keeping the patient in a fully upright posture and providing varying amounts of power to one or both legs. EksoNR uses a gyroscope, sensors, and software that monitors the position of the EksoNR to ensure that training is done effectively and safely. As a patient progresses and regains midline orientation, coordination, and strength, EksoNR will reduce the output of power allowing the patient to progress so they can walk out of the device.
The patients who use EksoNR exoskeletons post-stroke are kept apprised of their progress and must actively participate in the process to succeed. This might look like assisting with weight shifts, and may progress to the patient controlling all aspects of the steps they are taking. This involvement and positive progress reports can have a profound psychological effect on the patients, increasing their odds of improving outcomes.