Author: admin
10 Amazing Ways to Increase Patient Engagement
According to a survey conducted by NEJM Catalyst Insights Council survey [1], healthcare practitioners believe that only 34% of patients are engaged in the care process. This statistic is worrying, given that a huge part of a patient’s well-being is determined by their interest and participation in their health. Irrespective of the medical innovations and advancements, it takes effort from the patient to generate positive and sustainable outcomes. This can be compromised when patients are not engaged in the care process, hence the need for patient engagement.
Patient engagement can lead to better outcomes and improved long-term health. It can also reduce the cost burden on the healthcare system and reduce preventable readmissions. This article highlights ten efficient strategies you can implement now and their benefits.
What Is Patient Engagement?

Patient engagement is defined as the process where patients are actively interested and proactively participate in their own well-being. When carried out well, it becomes a shared responsibility by all stakeholders in the healthcare process, including the patients, healthcare workers, and administrators. The patient takes a keen interest in their health, healthcare workers involve the patient actively in the healthcare process, and the administrators facilitate the effective collaboration of healthcare professionals and the patient.
Patient engagement provides a platform for health workers to be more transparent and open, which translates into a responsive system. In other definitions of patient engagement, the engagement goes beyond education and decision-sharing. It includes training and financial support as a necessary means of aiding patient participation. This makes it clear that patient engagement isn’t only about getting patients engaged in the process but also inspiring healthcare organizations and workers to play a more active role.
How to Increase Patient Engagement

1. Create Patient Segments
All patients have different needs and diagnoses. Creating patient segments involves clustering all patients with similar conditions and needs within the same group. Creating patient groups can help you as a therapist to better understand patient needs and draw insight into the type of treatment that may work best. It can also help you create targeted strategies that will help you deliver better care to the individual groups. For instance, you can create a segment of patients with upper extremity mobility issues and another group for patients with lower extremity mobility issues instead of clustering them together. This will help patients gain peer support and community with other patients who understand their struggle.
2. Educate Patients
Education is a big part of patient engagement. Consider this; a patient walks into a medical facility for an appointment. They have no idea what’s going on with their body, only that they are experiencing different symptoms, and they are not well. They consult with a doctor and immediately receive a prescription for a medicine they are not familiar with, lifestyle adjustment recommendations they don’t understand, and a “get well soon.” This patient is more likely to disengage in their treatment and give up due to a lack of understanding. A patient with better knowledge of the prescribed medication and recommendations, in comparison, is more likely to follow the recommendations.
The American Journal of Medicine reports that 50% of patients with chronic diseases fail to benefit from treatment as a result of poor compliance which stems from low treatment understanding. [2] Lack of compliance normally leads to more hospitalizations, poor clinical outcomes, and reduced quality of life, making it essential to engage patients in order to increase compliance levels. A 2005 study reported that patients who received education materials were more compliant to treatment compared to those who did not receive educational materials. This resulted in more treatment satisfaction, increased communication with healthcare providers, and better outcomes. [2]
When educating patients, it is important to use clear language that your patients can easily understand. You can use handouts, website portals, and a teach-back method as part of your education strategies.
3. Involve Patients in Decision Making
One of the main areas that patients value in their interaction with physical therapists is shared decision-making. While they may not be vocal about it, research has shown that patients have better treatment outcomes when they are involved in decision-making. [3] I think we can agree that nobody likes being told what to do, but when involved in the decision-making process, we feel seen, heard, and considered. This applies to your patient interactions as well. While you may be the expert in the room, the patient is the expert on their routines, preferences, and body. Involving them in the treatment decisions will help you come up with better solutions that are suited to their individual situations.
A Mayo Clinic study showed that hospital admissions were reduced by 19% when they implemented a patient decision-making program. The researchers reported that the decision-making tool helped provide better care and improved clinical outcomes. [4] You can incorporate shared decision-making in your patient sessions by:
- Educating your patients about available options and how they play out in the patient’s lifestyle.
- Discuss goals and values with your patient.
- Deciding on treatment with your patient.
Before utilizing shared decision-making, it is important to understand your patient’s preference toward shared decision-making and involve them accordingly. You can use available shared decision-making tools like statin choice, PCI choice, or Rheumatoid arthritis choice, among others. Shared decision-making for physical therapists might involve selecting the best therapy exercises together with your patient.
4. Deliver Continuous Care
Patient care doesn’t end when a patient receives their prescription and walks out of your office. Continuous care (ongoing supervision) should be part of your patient encounters until they learn how to take care of themselves in a sustainable and healthy way. According to research, continuous patient care contributes to increased patient satisfaction and decreased hospital visits. It is also associated with an increase in preventative care. This can go a long way, especially for patients who suffer from chronic conditions like diabetes. According to a 2016 study, continuous care was reported to help patients with diabetes reduce their medical costs and health complications. [5]
Continuous care outside of your therapy sessions will help the patient maintain their improvement trajectory and also keep them ready for subsequent therapy sessions.
5. Simplify Medical Information
A major component of patient education (seen above) is simplifying information. Medical information can be complex, especially for people with no medical background. This is one of the biggest obstacles healthcare professionals must overcome when dealing with patient engagement.
It is extremely important to use simple language that the patient and caregiver understands. According to a study done by the National Institute of health, family caregivers deal with more healthcare issues than the patients because they are in charge of administering medication and other treatments. [6] This can be taxing if the caregiver doesn’t understand the information provided by the doctor. This makes it crucial to tailor your communication to the health literacy of your patient/caregiver. Avoid using medical jargon that may be confusing when giving instructions. When teaching your patient, remove as many medical terms as possible, replacing them with common language or explaining what the medical term means.
6.Use Images and Charts When Communicating
Visual aids are one of the amazing tools you can use in your practice in order to simplify information. They are also great as they are more memorable compared to written text. Visual aids can be in the form of images, diagrams, and videos. For instance, when conducting physical therapy, you could show your patient a diagram of the structures within the body and how the therapy treatment will affect them. Many home exercise programs include pictures or videos to help the patient recall what to do at home.
7. Do Not Make Assumptions When Communicating with Patients
It’s easy to assume that patients understand because you already know the information you are sharing with them. However, the concepts you are sharing may be unfamiliar to them. Additionally, their understanding of the information is shaped by their beliefs and backgrounds as opposed to science. This makes it essential to make sure that they accurately understand what you share with them from a scientific perspective.
8. Start Engagement Before a Patient Arrives
Gone are the days when you had to wait for patients to walk through the door in order to start engaging with them. With the advancement of technology, you can begin engaging with your patient before their appointment. You can use pre-visit tactics like appointment reminders and intake forms to start engaging with your patients before consultations. This will help them prepare accordingly and help you understand critical information about your patient that can help you prepare for the consultation session.
9. Stay Engaged Throughout Aftercare
Aftercare is follow-up care given to a patient after hospitalization or after a major procedure. Aftercare is an essential period for patients because this is the period when treatment really takes place. However, most patients ignore and misunderstand aftercare instructions which can lead to more complications and readmittance. According to one study, non-adherence to aftercare instructions can be up to 70%, especially if they are complex or demand a lifestyle change. [7] This normally leads to poor outcomes and even death in some cases. It is reported that there are approximately 125,000 deaths/year resulting from complications encountered as a result of non-adherence.
This makes it important for healthcare providers to simplify aftercare instructions and to follow up to ensure that patients stick to the recommended treatment. This can be through scheduled phone calls, emails, or texts.
10. Use Preferred Patient Channels
When improving patient engagement, it is recommended that you meet patients where they are, and this involves making an active commitment to reach out to them either before or after treatment. In order to do this effectively, it is recommended that you use their preferred communication channel. Potential channels you can use include: Whatsapp, email, phone, text, zoom, and patient portals. The list is endless here, but the most important thing is using a channel that the patient is comfortable engaging in.
Why Is Patient Engagement Important?
The importance of patient engagement cannot be overlooked. It is critical in improving healthcare standards, lowering cost, reducing wastage and improving patient outcomes, and well-being.
1. Improved Outcomes
One key benefit of patient engagement is improved patient outcomes. Active participation by patients increases their chances of adherence to treatment which equally contributes to better health. As pointed out above, non-adherence affects treatment outcomes, and patient engagement is the only way to reduce that.
2. Higher Quality Care
A quality gap exists in the healthcare system where healthcare processes differ from the outcomes achieved and observed. Patient engagement can help improve the quality of care, thereby closing this gap.
3. Improved Patient Satisfaction and Retention
Patients want to be seen, heard, and acknowledged. Engagement makes them more engaged in the treatment journey, resulting in satisfaction with the service they receive. This contributes to increased loyalty which can help you retain patients for longer.
4. Improves Patient’s Long-Term Health and Well-Being
When patients are engaged in their health, they are more likely to make better decisions that affect their health and well-being positively. When patients engage and become active, they are also more likely to detect disease symptoms early and seek treatment without putting it off (before it becomes a big issue).
5. Reduces Waste
More often than not, patients receive aftercare instructions in the form of flyers and pamphlets, but very few read them. This results in wastage. However, when similar materials are presented to engaged patients, they are used as expected, resulting in productive use, thereby reducing waste.
6. Reduces Potentially Preventable Readmissions (PPR)
According to this study, unengaged patients have higher chances of readmission due to failure to follow aftercare instructions. This results in complications that may lead to readmission and sometimes death. This can be reduced by engaging them throughout the process with the strategies we mentioned earlier.
7. Lower Costs
Unengaged patients tend to have higher no-show rates, delayed care incidents, and unmet medical needs, which can be taxing on the healthcare system. Medication non-adherence is also very expensive and increases the cost burden on health care systems.
According to research, patient engagement may lead to reduced costs within the healthcare system. The New England Healthcare Institute reported that the total estimated savings of this endeavor amount to over $290 billion in the U.S. Engaging patients also leads to better recovery, reduced no-show rate, and fewer visits. According to this 2018 study, non-adherence costs are avoidable, and one way to ensure this is through patient engagement. [8]
Conclusion

Incorporating the patient engagement strategies discussed here will increase treatment effectiveness, leading to higher patient satisfaction. Inadvertently leading to higher patient retention rates and more referrals to your practice. It can also help increase therapy completion rates.
While patient participation is vital in improving clinical effectiveness, it is important to remember that patient engagement goes both ways. It requires you to put in the effort during a patient visit and requires patients to put in more, if not the same, effort in contributing to their own well-being.
References:
1. Patient Engagement Survey: Improved Engagement Leads to Better Outcomes, but Better Tools Are Needed
2. Approaches to Patient Education: Emphasizing the Long-Term Value of Compliance and Persistence
3. Efficacy of Patient Activation Interventions With or Without Financial Incentives to Promote Prescribing of Thiazides and Hypertension Control: A Randomized Clinical Trial | Cardiology | JAMA Network Open
4. Shared Decision-Making Reduces Cardiac Admissions from the ED
5. Shared decision making in patients with low risk chest pain: prospective randomized pragmatic trial | The BMJ
6. Family Caregiving Roles and Impacts – Families Caring for an Aging America – NCBI Bookshelf
7. The challenge of patient adherence – PMC
8.Economic impact of medication non-adherence by disease groups: a systematic review – PMC
How Robotic Legs Can Support Paraplegic Conditions
Did you know that spinal cord and brain injuries are the most common cause of paraplegia, with spinal cord injuries affecting more than seventeen thousand people annually in America and brain injuries affecting up to 1.5 million per year? [1] A 2013 study done by Christopher & Dana Reeve Foundation revealed that about 1 in 50 people live with paralysis, nearly 5.4 million people. This is equal to the combined populations of Philadelphia, Los Angeles, and Washington, D.C. [2]
Despite the high number of people who need assistive devices like wheelchairs and walkers to move about and complete daily activities, little has been done to advance innovation in that field. That is, until the last decade when robotic legs (medical exoskeletons) were introduced in rehabilitation and recovery centers. Now, patients with paraplegia aren’t limited to a wheelchair, which may have access and mobility issues. This new innovation has led to the development of external robotic devices which can help enhance recovery through repetitive movement and improved neural plasticity. Additionally, they can serve as mobility support beyond walkers, wheelchairs, and orthoses. [3]
According to the Exoskeleton Industry 2019 Global Market research report [4], the increased uptake of exoskeletons in the medical industry has encouraged companies to invest more in research and development.
Are robotic legs the answer to helping people with spinal cord injuries, neurological disorders, and strokes regain independent function and their ability to walk again? In this article, we will break down what robotic legs are, the paraplegic conditions that are supported by robotic legs, the benefits of robotic legs, and where you can get them.
What Are Robotic Legs?

Robotic legs are powered medical exoskeletons that are fastened to the lower back and legs. They usually have motors and sensors attached to the hip and knee joints which coordinate and adjust with each step. Some robotic legs are customized to the wearer’s needs, allowing them to perform various tasks, including driving. To break it down further, a medical exoskeleton is any robotic system that patients with conditions like stroke, multiple sclerosis, brain injuries, and spinal cord injuries can wear to support movement.
Exoskeletons represent the coming together of man, machine, and work by responding to the user’s movement. They provide motor support to the wearer through patient-initiated movement or based on the setting the physical therapist uses and dependent on the patient’s needs.
Operating an exoskeleton is pretty easy for both you and your patient. The wearer only needs to shift their weight in the direction they want to move. The sensors then pick up the intended movement and offer support. With a powered exoskeleton, the wearer can stand from a sitting position, walk, and may even climb stairs. However, it is essential to note that these activities require training.
Robotic wearable technology has a wide range of applications and can be used by people with spinal cord injuries, brain injuries, multiple sclerosis, and stroke. According to Conor Walsh, a roboticist at Harvard University, “Robotic technology has recently expanded to benefit stroke patients. More than 70% of people who suffer a stroke never regain their full walking capacity.” At the same time, exoskeletons are not limited to medical uses only. They are also used by industrial workers like construction workers and warehouse workers to support the lifting of heavy loads. In fact, some companies have made it mandatory for workers to use exoskeletons as part of their personal protective equipment. They include: Ford, BMW, Hyundai, Samsung, and Mitsubishi, among others.
Paraplegic Conditions That Are Supported by Exoskeletons

One of the conditions we highlighted that is a common cause of paraplegia is spinal cord injury. When spinal cord injuries happen, they interfere with the communication between the brain and body parts below the injury, leading to paralysis. Exoskeletons can be used to support paralysis caused by spinal cord injuries, including injuries to the cervical, thoracic, and lumbar regions.[5]
To support this assertion, several studies have been conducted to investigate and verify the usefulness of exoskeletons for paraplegic conditions. In a 2018 study concerned with the development and control of a robotic lower limb exoskeleton for patients with paraplegic conditions, healthy subjects tested exoskeletons by performing normal daily activities like walking, standing, and sitting. It was concluded that the exoskeletons had natural gait cycles which support ambulation. [6] In simple terms, it demonstrated the exoskeleton’s ability to aid the rhythmic movement of a stride, which is needed in walking.
Exoskeletons have been shown to have a high impact on people with disabilities who were trying to regain muscle activity in their thighs, hips, and legs. In a clinical trial published in Frontiers in Robotics and AI, it is reported that 62% – 72% of wearers who practiced using exoskeletons in physical therapy could achieve their walking goals within 12 sessions. It also noted that after the 36th session, 80%-84% of the study groups achieved their walking goals. [7]
To demonstrate how useful and practical exoskeletons are in patients’ recovery and daily activities, here are two stories of patients who rely on exoskeletons.

At 22 years old, Julio Caro, a structural steelworker in southern California, took an 18ft fall while working, which would change his life forever. He broke his back in two different places, injured his spine, and was unable to walk after the ordeal.
“I was young, and so I didn’t understand what was happening,” Caro said. “They said, ‘You’re not going to be able to walk again,’ and I thought they were lying.”
“I just wanted to get back on my feet — I was out to prove everybody wrong,” he added. “So when I first heard [about exosuits], I was, like, Robocop. As soon as I saw the machine and I saw it walk, I thought, ‘Oh cool, it does everything for you.’”
After using the exoskeleton for only five sessions in physical therapy, Caro was able to walk again. He says it made a lot of difference having the robotic legs as they allow him to work again and enjoy what we might typically take for granted, like reaching out and touching a leaf.
“I’m glad this technology is out there, [and] it’s only getting better,” he added.

On Tuesday, December 4th, 2018, Amelia Clark dropped off her three sons at school and went to a hair-coloring class. She had a headache but thought nothing of it. She dismissed it as low blood sugar until the unthinkable happened. She couldn’t stand up.
“I must have passed out because when I woke up, I saw a whole bunch of lights, and the doctor said, ‘Hi. What’s your name? You’ve had a stroke.’”
Clark was hospitalized for a month and a half, unable to walk without any assistance. The first time she took a step after her stroke was when she was introduced to an exoskeleton, EksoNR. In just three months, she was able to walk with a cane and, by August, started driving again.
Benefits of Robotic Legs

- Robotic Legs Don’t Require Surgery
One great thing about robotic legs for physical therapy patients is that, unlike other treatments, they don’t require invasive surgical procedures. For instance, in epidural stimulation, a device is implanted near the spine, and in stem cell transplants, spinal cord injections are done. Conversely, robotic legs (exoskeletons) are worn on the body, making them an easy way to improve mobility without risk of complications.
- Robotic Legs Improve Circulation
When you have a spinal cord injury, blood tends to pool in the legs due to lack of movement, reducing the amount of blood flowing to the heart. It can also lead to swelling in the legs. Using exoskeletons can allow your patients to ambulate and move paralyzed areas. This contributes to the circulation of blood which is essential in supporting cellular activity.
- Robotic Legs Reduce Muscle Atrophy
Movement is very critical as it helps in strengthening muscles and bones. However, patients with paraplegic conditions may not be able to move around much. This can cause their muscles to reduce in size to conserve energy, hence the need for robotic legs. Though they do not stop muscle atrophy, they help maintain bone and muscle density as they keep the wearer moving and bearing their own weight.
- Robotic Legs Boost Confidence
When a patient experiences an injury or condition that affects their lower limbs, the recovery outlook is painted as marginally lower, and this can impact patient confidence. One of the most invaluable benefits of robotic legs is the hope they restore to patients who’ve been told they’ll never be able to walk again. Robotic legs represent an opportunity for them to walk again, which not only helps them become more independent but also more confident. Robotic legs can be used for rehabilitative exercises and help patients with complete SCI regain more mobility than they thought possible.
- Robotic Legs Help Manage Spasticity
One of the most common problems that patients with paraplegia face is a painful condition known as spasticity (the contraction of muscles). Robotic legs can help manage spasticity and improve other related conditions like pain and bowel function. When one robotic leg user was asked, she said that tending to her bowels took roughly 20 minutes, which was different from the hour she usually spent without an exoskeleton. [8]
The Best Robotic Legs for Paraplegic Conditions

There are different types of exoskeletons available in the market for paraplegic conditions that assist physical therapists, additionally, these exoskeletons have been approved for use in communities and medical institutions with supervision. One great example is Ekso Bionics’ EksoNR which is used to rehabilitate people after spinal cord injury, stroke, brain injury, and MS.
The EksoNR is like a backpack that extends to the legs and supports the torso and lower limbs. It has sensors on the footplates which signal the movements of the wearer. The exoskeleton then creates feedback and offers support to the wearer, depending on the settings. It not only supports ambulation but also helps patients regain muscle activity.
Where Can You Get Robotic Legs?

Robotic legs like the EksoNR and EksoGT are readily available in more than four hundred rehabilitation centers globally. If you’d like to acquire exoskeletons for your facility, you can contact our sales team by clicking here.
Conclusion

Robotic legs are essential for patients with paraplegic conditions. They help support movement, reduce muscle atrophy, and address other related conditions like pain, bowel function, spasticity, and overall quality of life.
Ekso Bionics has been at the forefront of creating the best quality medical exoskeletons for over a decade. Our EksoNR was one of the first FDA-approved medical exoskeletons for rehabilitation, and it continues to be the exoskeleton of choice for rehabilitation clinics. Please review our indications for use to determine eligibility. [9]
References:
- https://www.cdc.gov/traumaticbraininjury/pubs/tbi_report_to_congress.html#:~:text=Traumatic%20brain%20injury%20(TBI)%20is,people%20are%20hospitalized%20and%20survive.
- Paralysis statistics – Reeve Foundation https://www.christopherreeve.org/living-with-paralysis/stats-about-paralysis
- Robotic Rehabilitation and Spinal Cord Injury: a Narrative Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6095795/
- Exoskeleton Market Size & Share Report, 2022-2030 https://www.grandviewresearch.com/industry-analysis/exoskeleton-market
- Robotic Rehabilitation and Spinal Cord Injury: a Narrative Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6095795/
- Development and control of a robotic lower limb exoskeleton for paraplegic patients https://journals.sagepub.com/doi/abs/10.1177/0954406218761484?journalCode=picb
- How Exoskeletons Can Help People With Paraplegia Walk Again https://eksobionics.com/how-exoskeletons-can-help-people-with-paraplegia-walk-again/
- Robotics are helping paralyzed people walk again, but the price tag is huge – The Washington Post https://www.washingtonpost.com/news/morning-mix/wp/2017/06/10/robotics-are-helping-paralyzed-people-walk-again-but-the-price-tag-is-huge/
- Indications for Use – Ekso Bionics https://eksobionics.com/indications-for-use/
8 Patient Concerns All Therapists Should Know!
Physical therapy can be intimidating for patients, especially if they don’t have enough information, are afraid, or don’t have any prior experience with therapy. Misinformation and fear can lead to concerns and notions, which, if not addressed, can keep patients from seeking the help they need in order to recover well. It is important for therapists to understand their patients’ concerns to address them and increase patient safety. In this article, we will address the most common concerns patients have about physical therapy and how you, as a physical therapist, can address them to ensure patient safety and comfort.
Common Concerns Patients Have About Physical Therapy

- Some Patients Are Afraid of Pain
One of the most common misconceptions people may have about physical therapy is that it is painful. However, contrary to popular belief, physical therapy is actually designed to help relieve and manage pain, as you already know. Sometimes it takes explaining to patients the benefits of therapy in pain management and alleviation for them to understand how it works and what they should expect from it. Many people fail to realize that though therapy can be uncomfortable, it is never meant to be painful.
- Patients May Think Physical Therapy Is Time-Consuming
Time is generally a primary concern for most people. Most patients usually have school, careers, family, and other demands on their time. Therefore, when it comes to scheduling time for physical therapy, it can seem impossible to add one more thing to their already packed schedule. On the other hand, some patients may be concerned that physical therapy will take too long. They do not want to commit weeks and months of their time to attend therapy. When you consider the busy lives we lead and how we try to fit everything into our limited schedule, you can begin to empathize with your patients and understand where they are coming from. A great solution would be creating a rehabilitation schedule that is tailored to your patient’s schedule. It can include at-home exercises and in-office rehabilitation sessions.
- Patients May Believe Physical Therapy Is Too Expensive
Physical therapy is not familiar to most people. It’s not a program your patient may have undergone before, and people tend to be afraid of the unknown. This can be a barrier for many patients. Additionally, if your patient does not have insurance to cover their costs, paying out of pocket can be too expensive. However, you can work with patients to discuss cost-cutting strategies they can leverage to get the treatment they need.
- Some Patients Are Afraid That Physical Therapy Won’t Work
How do you know something is going to work, especially if you have never experienced it before? This is the same thought that may plague patients, as they may not ascertain the effectiveness of attending therapy sessions. This might be less of a concern for patients who have undergone rehabilitation before, but it can be a very real concern for patients who haven’t undergone physical therapy. To curb this, you can share success stories with your patients that qualify the importance of therapy during consultations.
When someone is suffering from mobility issues, it might be easier to convince themselves that rehabilitation won’t work rather than have hope and then get discouraged. Getting over this mental barrier may help some patients open up to physical therapy.
- Some Patients May Be Afraid of Working With a Physical Therapist
Even though therapists normally try to be friendly and welcoming to everyone, sometimes some patients may feel uncomfortable and even afraid to do physical therapy. This may be due to personal issues like haphephobia (the fear of being touched by strangers) and uncommunicated expectations like the outcome they desire out of physiotherapy.
- Patients May Be Afraid of Commitment
Just like going to the gym or starting a new diet, physical therapy comes with a demand for commitment; not many patients feel they can stick it out till the end. This may keep many patients from trying because they already believe they will fail. However, working out therapy plans that work for your patients can help them conceptualize how much will be asked of them within the program. This can help them evaluate their commitment using a tangible measure compared to going at it blindly.
- Some Patients Are Afraid of Falling
Some patients are concerned about attending therapy because of the fear of falling, clinically referred to as “ptophobia”. According to Tinetti of the Department of Medicine and Public Health at Yale University and Powell of the Department of Epidemiology and Public Health, the fear of falling (FOF) is an ongoing concern about falling that ultimately limits the performance of daily activities.[1] Reduced mobility makes patients insecure about avoiding falls, effectively keeping them out of therapy.
- Patients May Be Afraid of Getting Injured
Sometimes patients incur injuries during physical therapy sessions due to falls, among other reasons. This can keep prospective patients from going to therapy as they are afraid that they’ll meet the same fate. Reassuring your patients can go a long way in overcoming this fear. Addressing patient safety is a key concern in ensuring that patients are safe within rehabilitation facilities. This might go a long way in relieving patients’ fears.
In the next section, we’ll discuss patient safety and how physical therapists can ensure they observe patient safety guidelines to ensure their patients get the best care and treatment.
How to Address Patient Concerns as a Therapist

There are a few things you can do to deal with your patient’s concerns, including:
- Understand Your Patient’s Needs
The most significant step you can take in addressing your patient’s concerns is understanding their needs. A lot of patients have different needs and concerns that can only be met if you are empathetic and understanding enough. Addressing these needs can be the start to relieving any anxiety and worry that a patient has. It can also be the foundation of trust that you need to form with a patient in order to help them through their therapy sessions.
- Create a Rapport With Your Patient
This will help them to open up and be more active in therapy sessions. Building a relationship with patients is the fastest way of getting them out of bed. A 2010 study studying the influence of the therapist-patient relationship on treatment outcome in physical rehabilitation said that the connection between a therapist and patient determines the treatment outcome. [1]
- Communicate and Address Expectations Clearly
Effective communication is a primary facet of successful rehabilitation. Communication is needed to understand your patient’s needs and expected outcome. While communicating with your patients, it’s also important to tailor your communication to your patient’s literacy level when discussing ailments and treatment. Patients value clear and simple explanations about their problems.
Addressing Patient Safety

Patient safety has become an evolving area in the healthcare industry with the increase of adverse events in hospitals. Adverse events are any unintended occurrences within the healthcare system that may lead to a longer hospitalization period, disability, or death.
According to the Canadian Patient Safety Dictionary, patient safety is “the reduction and mitigation of unsafe acts within the healthcare system, as well as through the use of best practices shown to lead to optimal patient outcomes.” [2] Physical therapists play an important role in mitigating unsafe acts within the system, directly and indirectly. Physical therapists can contribute to a culture of safety by evaluating and implementing safety measures like improving facility layouts, training staff, and being more sensitive to patients’ needs, among others, as discussed below.
Safety issues within physical therapy are not typically big and harmful events. They are normally no-harm events classified as close calls or near misses. In other words, they are events that happen to the patient but do not produce harm. For example, a patient almost falls when they are being moved from a chair. These kinds of events happen as mistakes, and it is important to identify the source of these mishaps and learn from them so as to improve patient safety. [3]
According to a 2004 study by the Canadian Medical Association Journal, some of the adverse events that normally happen in the health care system can be prevented altogether. [4] So, let’s explore some strategies you can implement to mitigate against accidents in your practice and improve patient safety.
How to Increase Patient Safety as a Therapist

You can implement several strategies to alleviate your patient’s concerns. They include:
- Identifying Potential Slip and Fall Risks
This is one of the easiest things you can do to increase safety in your facility. Injured patients are vulnerable to falls and slips, so it is extremely important that you ensure slippery areas are shown well. Additionally, you can station staff in risky areas to watch patients during their visit to your practice. Also, never forget to notify patients in case you identify potentially risky areas where they may fall and injure themselves. It is also important to wipe and clean any spills immediately to avoid the risk of a fall. And if your facility has bathing areas, make sure they are always kept dry to avoid injuries. Additionally, you can add non-slip rugs in the bathrooms and grab bars for support.
- Improving the Facility Layout
Evaluate your facility to see if patients can easily move from one area to another without straining and injuring themselves. Remember that a good number of patients attending therapy have mobility issues. A great solution to ease patient movement would be having ramps around the facility instead of stairs. You could also place all equipment and furniture out of the way of patients to avoid any falls.
- Making Signage and Posters Visible
Having signage and posters all over your facility is great, but they need to be visible and legible. What good is a warning poster if a patient can’t see it or be able to read it? The United States Occupational Safety and Health Administration dictates that all labels, posters, signs, and color codes must be visible enough to warn patients of possible risks.
- Labeling Equipment and Providing Instructions of Use
As great as equipment exercise is, it can pose a potential hazard to patients if it does not have any clear instructions for use. Instructions are normally included in any equipment you buy, but in case it is not, make your own and make sure it is visible enough to be seen by the patients using it.
- Training Staff
The best way to increase patient safety and improve healthcare quality is to train staff on the latest and best ways to take care of patients. Additionally, creating a work culture that puts patient safety first can also help address patient concerns like safety.
Conclusion
Patient concerns are ever-changing and differ from one patient to another. If left unchecked, they can keep potential patients from attending therapy and getting the help they need. When addressed, they can help patients overcome their personal barriers and attend physiotherapy sessions.
When dealing with patients, it is important to remember that you are human, and humans make mistakes. Whenever a mistake is made, the best course of action is to learn from it and make the required changes. It is also important to create a culture and environment that facilitates the identification and reporting of mistakes so that you can improve patient safety.
References:
- Fear of Falling | Physical Therapy | Oxford Academic https://academic.oup.com/ptj/article/82/3/264/2837020
- The Canadian Patient Safety Dictionary https://policycommons.net/artifacts/1212508/the-canadian-patient-safety-dictionary/1765612/
- Patient Safety and Physiotherapy: What Does it Mean for Your Clinical Practice? https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2909853/
- The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada https://pubmed.ncbi.nlm.nih.gov/15159366/
5 Best Physical Therapy Types For Postoperative Patients
Postoperative therapy is a big part of the recovery process and is necessary to restore joint movement, strength, and flexibility. It might be required after surgical procedures like orthopedic, cardiac, thoracic, neurological, and abdominal surgery. Many patients may prefer skipping this step of their recovery, but this can result in improper or incomplete healing.
Postsurgical therapy is helpful if you are experiencing stiffness, pain, muscle weakness, reduced mobility, reduced balance, and reduced coordination. It also helps with any physical and psychological effects you may have endured due to surgery.
According to a National Institutes of Health (NIH) study, patients who stay in bed after surgery tend to lose muscle strength, heart capacity, and lung capacity due to a lack of physical activity. [1] But with the incorporation of physical therapy in recovery, you can prevent functional atrophy. This article will explore the phases of postoperative rehabilitation, types of physical therapy, and the benefits of postoperative rehabilitation.
The 3 Phases of Postoperative Rehabilitation

There are three main phases in postsurgical rehabilitation, and they differ from patient to patient depending on the type of surgery. They are broken down into:
- Stage 1: In this stage, you’ll be immobilized as you’ll be fresh from the surgery room. Typically, you’ll be in pain, and the surgical area will be swollen. At this point, rest is recommended for a few hours or days, depending on the type of surgery.
- Stage 2: In this stage, the pain and swelling will reduce. You’ll be able to move a little and will be ready to start physical therapy. The goal, at this point, is to strengthen the body, improve stability, and restore range of motion.
- Stage 3: In this stage, you’ll be continuing to heal and are ready to rehabilitate and learn to complete your activities of daily living. The ultimate goal of physical therapy will be achieved in this stage.
Surgery Operations That Require Postoperative Physical Therapy

These are five surgical procedures that necessitate physical therapy as part of the recovery process. They include:
- Brain tumor surgery: A 2019 pilot study on the effectiveness of rehabilitation therapy after brain tumor surgery reported that intensive rehabilitation resulted in improved motor function, cognition function, and Activities of Daily Living (ADL). [2] In this case, physical therapists focus on range-of-motion exercises, balance, gait, and endurance training.
- ACL and Meniscus Repair: ACL knee ligament and meniscus cartilage repair is a problem often associated with athletes. According to a 2019 study conducted by the International Journal of Sports Physical Therapy, physical therapy is vital in hastening the healing process and avoiding re-injury. Physical therapists usually focus on building quadriceps and hamstring strength in the recovery process. [3]
- Back and Spine Surgery: Physical therapy is vital, especially because of the delicate nature of spinal surgeries. Your physical therapist will show you exercises and movements for your back that don’t put pressure on your spine. Therapy strategies normally include stretches and exercises that get the blood flowing. In the case of more invasive surgeries, for example, spinal fusion, your therapist can monitor your back health and update your doctor on the healing progress.
- Heart Attack/Bypass Surgery: According to a 2018 study by the Journal of Physical Therapy Science, preoperative physical therapy can help prevent cardiopulmonary complications by offering patients a safe space to move. Low-impact exercises tend to improve health and reduce your stay in the hospital. Coupled with postoperative therapy, you can recover faster while avoiding all postsurgical complications. [4]
- Achilles Tendon Release (Tenotomy): This is a type of surgery that is done to fix a damaged or contracted Achilles tendon. This procedure can be performed to relieve shortened and stiff muscles to allow for better range of movement. This is a common problem for patients with spinal cord injuries because, after a spinal cord injury, the normal flow of nerve signals is disrupted and feet tend to relax into a toe-pointed position. This could limit a person’s ability to stand if not corrected.
Major Types of Physical Therapy For Postoperative Patients
Physical therapy strategies are not one-size-fits-all. The type of therapy recommended always depends on your physical condition and biomechanical needs. In this section, we will explore rehabilitation methods that are applicable to patients who have undergone any kind of surgery.
- Stretching
After surgery, the soft tissue normally contracts, and scar tissue forms. This can decrease flexibility and make it difficult for you to move. However, regular stretching can help prevent immobility caused by scar tissue. It also helps increase joint flexibility and a full range of motion in case of joint surgeries. Overall, stretching makes life much easier and allows you to do simple tasks like reaching over your head, walking, and even climbing stairs.
Stretching has also been shown to help improve balance and reduce pain by relaxing tense or spasming muscles. Lower back, abdominal, hip, and leg muscle stretches are recommended if you’ve undergone back surgeries.
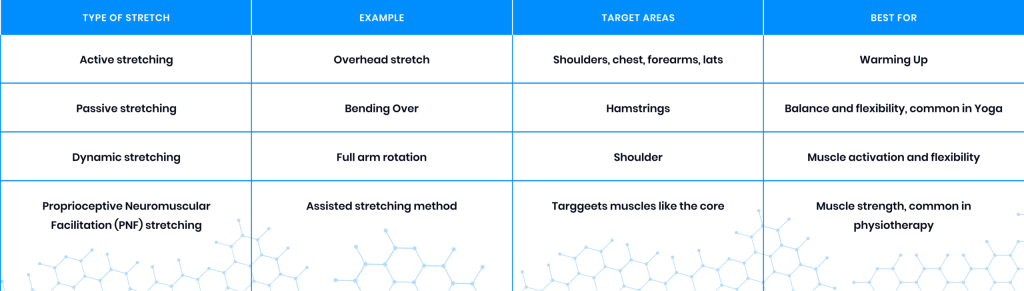
Common hamstring exercises targeting the outer hip and lower back include Knee to Chest Stretch, Figure 4 Stretch, Pigeon Stretch, and Doorway Hamstring Stretch. These stretches are particularly great for tight and restricted muscles. The Pigeon Stretch and Doorway Hamstring Stretch are more advanced and should only be performed in a pain-free range. Other types of stretches used in postoperative therapy include:
- Range of Motion Therapy
Range of motion (ROM) is concerned with how far you can move an affected joint or limb in all directions and positions naturally without strain and pain. There isn’t one standard definition of ROM. According to Dr. Aldalbert Kapandji, who specializes in physical therapy, range of motion is “the extent of osteokinematic motion available for movement activities, functional or otherwise, with or without assistance.” [5]
Range of motion exercises increase movement, reduce pain, and improve joint integrity and function. Range of motion exercise and stretching are generally performed in the first phase of rehabilitation to help regain joint functionality before moving to more advanced practices.
Range of motion therapy normally includes:
- Passive routines where the therapist guides your movements.
- Interactive routines where both you and the therapist do the work.
- Active routines where you do the exercises on your own.
Range of motion exercises involving circling joints and knee extensions are beneficial in different situations, including:
- Soft tissue and joint recovery
- Joint and soft tissue mobility
- Neuromuscular reeducation
- Synovial movement enhancement
- Strengthening
Strengthening exercises are a crucial part of physical therapy and help improve muscle function around the surgical area. Strengthening exercises are customarily performed alongside or after the range of motion exercises because increased joint movement without an equal increase in strength might cause injury.
Strengthening exercises are also vital in improving your core strength. The core is a major focus area because it is the source of stability. Rebuilding core strength improves stability and mobility and helps prevent additional injuries. It allows you to increase the load you can handle without overexerting and injuring yourself. In addition, strengthening can also be used for the back and pelvis areas. Strengthening exercises typically include leg raises, hamstring and quadriceps contractions, and squats using a chair.
Strengthening exercises can also include bridge exercises and ball bridge exercises. These exercises are great for strengthening the hamstring, lumbar extensor, pelvic, back, and buttocks. These exercises should be done in a pain-free range; once you’ve mastered them, you can move on to more advanced strengthening exercises.
- Ultrasound and Electrical Therapy
Ultrasound and electrical therapy help improve blood flow and retrain nerves. Ultrasound therapy involves the use of high-frequency sound waves on deep tissue. The high-frequency sound waves used to stimulate deep tissue are so low that even the human ear cannot pick them up. This type of therapy utilizes a probe for administration and is known to reduce pain, accelerate healing, and reduce inflammation in the soft tissues. A 2014 study conducted by the Journal of Physical Therapy Science reported that therapeutic ultrasound increases range of motion and pain threshold for at least 20 minutes. [6]
Electrical therapy involves the use of low electrical current on the deep tissues. Electrical stimulation works by sending small electrical currents to the targeted area and the nerves surrounding it. It is extremely helpful in increasing blood flow, pain management, and improving muscle flexibility. A 2021 study conducted by Frontiers in Medicine reported, “As a supplementary treatment after total knee arthroplasty, postoperative neuromuscular electrical stimulation could improve the short-term to long-term quadriceps muscle strength, mid-term pain, and mid-term function.” [7]
- Gait Training
Walking is a great physiotherapy technique that’s primarily used for neurosurgery patients. It normally involves rewiring and training the brain to control walking muscles. This is achieved because of the brain’s neuroplasticity – the ability of the brain to form and reorganize synaptic connections. When walking is practiced regularly after surgery, it allows the brain to strengthen and create neural pathways that support movements involved in walking. Some high repetition walking exercises include leg and balance exercises.
Benefits of Postoperative Therapy

General Surgery
A postoperative therapy program after general surgery is a crucial part of recovery and offers a host of benefits like:
- Proper Healing and Faster Recovery Time
Many complications can arise after surgery, including infection and muscle atrophy, which might lead to poor healing. That’s why postoperative therapy is important. Postoperative therapy can help wounds heal properly by minimizing scar tissue, retraining muscles, and recovering joint function. It also allows you to enjoy a faster recovery time. According to a 2017 study conducted by Acta Medica, beginning physical therapy following a joint replacement surgery can reduce your hospital stay and help you recover faster. [8]
- Patient Participation
Patients who actively participate in their own recovery process have been shown to have better results and recovery experiences than those who don’t in a 2013 review conducted by researchers from the Health Policy Research Group at the University of Oregon. [9]
- Improves Mobility
Joint replacement surgeries normally result in reduced mobility, making activities that may seem ordinary, like walking, difficult. This happens because of the body’s natural response, which is to protect the area of surgery by swelling, reducing the range of motion, and tightening the muscles. This makes physical therapy extremely important, especially after knee and hip replacement surgeries, as it may help you recover your mobility through targeted postoperative therapy practices.
- Eases Pain and Swelling
Swelling and pain after surgery normally vary from one person to another. The pain usually arises when chemicals that stimulate nerve endings are released, and the excess inflammation compresses the nerves. Exercises are a great tool for reducing swelling, which results in improved mobility, faster healing, and reduced pain. Postoperative physical therapy administration can also help in preventing chronic pain.
According to a 2013 review conducted by London-based medical researchers, postoperative therapy is quite effective in improving short-term lower back pain and long-term lower back and leg pain if you’ve undergone lumbar spinal stenosis surgery. [10]
- Reduces Scar Tissue Formation
During the healing process, scar tissue forms, and tissues contract. This normally leads to scarring and reduced mobility. However, mobilization techniques can help prevent this using ultrasound therapy, which effectively increases flexibility and softens the scar tissue. According to a 2016 study conducted by researchers for the Internal Medicine Review journal of Washington D.C., low-intensity therapeutic ultrasound can help treat soft tissue injuries and improve musculoskeletal and post-operative recovery outcomes. [11]
- Reduces the Development of Secondary Issues
Physical therapy can help reduce surgical complications like blood clots, and infection, among others. Specific exercises and movements may help in reducing the risk of contractures and other complications.
- Improves Flexibility
Staying in bed after surgery is detrimental for you, and it may lead to weak muscles, which will make you susceptible to injury. When your joints become stiff, activities like walking, climbing stairs, and reaching overhead can be compromised. However, stretching exercises can help you keep your joints flexible and muscles limber.
Neurosurgery
Neurosurgery is involved with the treatment of conditions affecting the nervous system, including the spinal cord, brain, and peripheral nervous system. This makes postoperative rehabilitation very important as part of helping a patient regain their pre-surgery functionalities. Benefits attributed to physical therapy include:
- Increased Range of Movement – Patients are able to increase their limb and joint movement in any direction without any pain.
- Improved Gait – Physical therapy can help you improve your balance, coordination, and walking movement control.
- Increased Muscle Strength – Physical therapy is great for training leg and back muscles to support the weight of the body.
- Reduced Spasticity and Contractures (Shortened Muscles) – Surgery may lead to muscle tightness, otherwise referred to as spasticity, which can limit movement and cause pain. But physical therapy can help you avoid these complications.
Conclusion
Postoperative therapy is vital when you are recovering from surgery, and its efficacy has been shown in different studies. It will help you heal faster, regain mobility, reduce pain, and prevent postoperative complications. In case you’ve undergone surgery, physical therapy will offer you the recovery support you need on your healing journey.
References:
- Assessing the effectiveness of routine use of post-operative in-patient physical therapy services https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5506300/
- Intensive Rehabilitation Therapy Following Brain Tumor Surgery: A Pilot Study of Effectiveness and Long-Term Satisfaction https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6509576/
- Restoring knee extensor strength after anterior cruciate ligament reconstruction: a clinical commentary https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6350662/
- Prevention of postoperative pulmonary complications through preoperative physiotherapy interventions in patients undergoing coronary artery bypass graft: literature review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6110234/
- The clinical evaluation of the upper limb joints’ function: back to Hippocrates https://www.sciencedirect.com/science/article/abs/pii/S0749071203000295?via%3Dihub
- Effects of Therapeutic Ultrasound on Range of Motion and Stretch Pain https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4047237/
- Effect of Neuromuscular Electrical Stimulation After Total Knee Arthroplasty: A Systematic Review and Meta-Analysis of Randomized Controlled Trials https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8677678/
- Early rehabilitation after elective total knee arthroplasty https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6357664/
- What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs https://www.ncbi.nlm.nih.gov/pubmed/23381511
- Rehabilitation following surgery for lumbar spinal stenosis – McGregor, AH – 2013 | Cochrane Library https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009644.pub2/abstract
- Low-Intensity Ultrasound for Promoting Soft Tissue Healing: A Systematic Review of the Literature and Medical Technology https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6128661/
Why Physical Therapists Should Use Exoskeletons For Spinal Cord Injury Rehabilitation
According to the World Health Organization (WHO), between 250,000 and 500,000 people suffer from spinal cord injuries (SCIs) every year due to blunt force trauma, road crashes, falls, and other mechanisms of injury. [1] A few years ago, this would have meant the end of autonomy and mobility for many people, but thanks to advances in technology, there are more rehabilitation therapies available, including exoskeletons. The FDA designates medical exoskeletons as a class II (intermediate risk) medical device, and they are cleared for use with patients who have an SCI. [2]
Exoskeletons give people with spinal cord injuries a chance to ambulate, exercise, and engage in mobility and autonomous activities. In this article, you’ll learn what exoskeletons are, how they operate, and how they can be beneficial in physical therapy for patients with spinal cord injuries.
What is a Spinal Cord Injury (SCI)?
According to the National Institute of Neurological Disorders and Stroke (NINDS), a spinal cord injury is “damage to the tight bundle of cells and nerves that sends and receives signals from the brain to and from the rest of the body.” [3] SCIs could be a direct result of damage to the spinal cord itself, such as from a gun shot wound, but could also result from damage to surrounding tissues and bones that then compress the spinal cord. These injuries can permanently or temporarily affect mobility, sensation, and other body processes. Depending on the extent and location of the damage to the spinal cord, patients may experience some form of paralysis and/or sensory deficits that could be improved through rehabilitation, potentially leading to full recovery.
The most common causes of SCI are grouped into traumatic and non-traumatic causes. Traumatic SCI causes may include car accidents, falls, and sports-related accidents. Non-traumatic causes include tumors, neurodegenerative diseases, infections, and genetic causes.
Rehabilitation Methods Available for Patients with Spinal Cord Injury
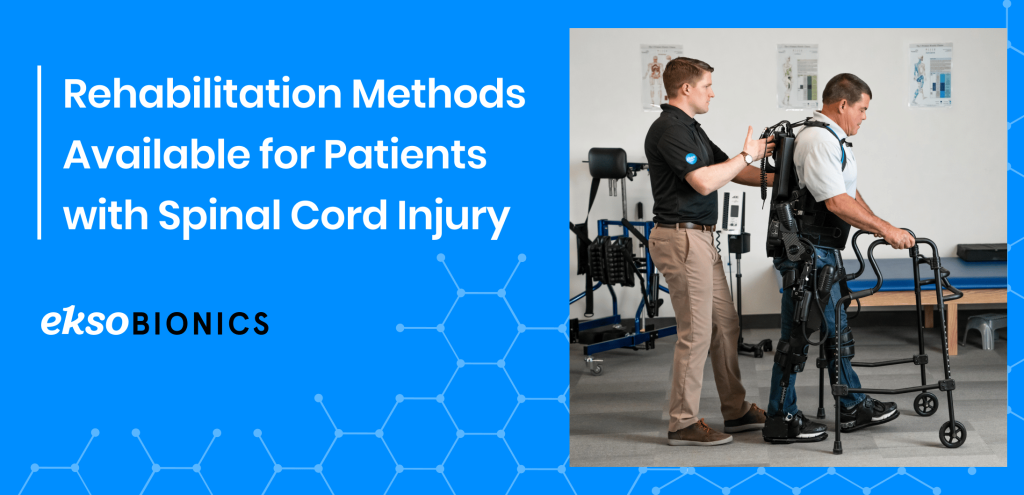
Rehabilitation therapies for patients with a spinal cord injury depend on the extent of damage and the type of injury. Patients usually start in the intensive care unit, followed by acute care, inpatient, and outpatient rehabilitation. Some hospitals even have a spinal cord injury department that specializes in this type of rehabilitation. This can last anywhere from three to twelve months or more, depending on the severity of the injury. Popular rehabilitative techniques include:
- Range of Movement, Strength, and Stretching Exercises
Spinal cord injuries limit the range of movement by causing joint immobility and flexibility issues. However, this can be remedied using stretching and strength exercises. According to a 2020 study, range of movement exercises help “prevent contractures, protect tenodesis effect, strengthen paralyzed muscles, promote nerve and cerebral remodeling, and improve spinal microenvironment and functional prognosis.” [3]
- Functional Electrical Stimulation
Functional electrical stimulation works by artificially stimulating the sensory-motor systems using electrical pulses. It activates neural pathways, which stimulate the muscles and cause movement. This therapy is used alongside other rehabilitation methods in order to restore mobility. According to a study, this procedure also “provides cardiorespiratory fitness; improves posture and trunk stability; prevents contractures, pressure ulcers, and orthostatic hypotension; promotes nerve restoration; and prevents peripheral nerve deterioration.” [4]
- Epidural Electrical Stimulation (EES) of the Spinal Cord
In this procedure, a device is implanted over the spinal cord’s dura mater through a laminectomy. It then produces a rhythmic electric pulse to the posterior nerve roots, which activate the central circuits which are responsible for regulating pain, movement, and the cardiorespiratory system. EES is beneficial for reducing fatigue, improving cardiovascular fitness, increasing body mass, and improving urination in patients. [4] However, this is not a simple procedure, as patients must undergo surgery for the device to be implanted and is not yet widely available.
- Transcutaneous Electrical Nerve Stimulation (TENS)
TENS utilizes a high and low electrical stimulation to the nerve to manage pain. It may also help with proprioception, balance, and spasticity. This method is very affordable, and patients can do it by themselves without much assistance.
- Occupational Therapy
Occupational therapy focuses on improving the physical, sensory, and cognitive functions of the patients. It helps patients suffering from SCI regain their autonomy and independence. It focuses on the execution of daily activities like grooming, bathing, cooking, and dressing, among others. Occupation is the gateway that helps patients attain inclusion and total adaptation to their environment.
- Robotic Exoskeletons
Wearable robotics, also known as robotic exoskeletons or exosuits, are a recent development in the healthcare industry that present unlimited potential for patients with spinal cord injuries and are used in conjunction with physical therapists. Robotic exoskeletons are used in rehabilitation to help in mobility recovery through repeated movements that lead to increased neural plasticity. [5] Exosuits offer benefits like improved gait, better life quality, improved moods, and better bladder control, among others, as discussed below.
According to Dr. Chester Ho, Associate Professor at the University of Calgary’s Department of Clinical Neurosciences and member of the Hotchkiss Brain Institute, introducing robotic exosuits early in a patient’s rehabilitation process offers better chances of recovery. He says, “The first nine months after a spinal cord injury are pivotal to recovery, so we want to attempt to introduce rehabilitation and mobilization early on and see if it makes a difference.” [6]
What Is An Exoskeleton?
Exoskeletons, first developed in 1890, are wearable electromechanical devices that support joint movement while enhancing the wearer’s strength and ambulatory capabilities. An exoskeleton frame is made to surround the waist and other joints like the shoulders and knees. Exoskeletons can be classified into two types: active, powered by an external power source; or passive, powered by mechanical springs and counterbalance forces.
Exoskeletons are used in physical rehabilitation clinics to promote a patient’s mobility and increase their muscle strength. They do this by allowing for repeated movements that increase neural plasticity and help develop mobility. [4] The use of exoskeletons in physical therapy is reported to increase “quality of life, body composition, bone density, neuropathic pain, spasticity, gait speed, number of steps, and distance before and after 90 days of training.” [4]
How Are Exoskeletons Controlled?

Exoskeleton control is vital in a physical therapy environment. Exoskeletons offer multiple control modes, and operators can choose the amount of resistance that is applied at the joints. Exoskeletons can be controlled by the patient or physical therapist depending on the degree of patient recovery. Control methods include: [7]
- Sensors: Sensor-controlled exosuits have numerous sensors fitted into the build that capture nerve signals and control torque, pressure, tilt, and rotation.
- Buttons/control panels: Some exosuits contain pre-programmed modes, which are normally controlled by the user or by the physical therapist. Most control panels are located on the walking aids.
- Joystick: This is commonly found in active exosuits that provide all the energy required by the wearer.
- Mind-Controlled: These use an electrode skull cap as the main method of control.
No-control: Most passive exosuits do not have control buttons and respond to the mechanical movements of the wearer.
Exoskeleton control is vital in a physical therapy environment. Exoskeletons offer multiple control modes, and operators can choose the amount of resistance that is applied at the joints. Exoskeletons can be controlled by the patient or physical therapist depending on the degree of patient recovery. Control methods include: [7]
- Sensors: Sensor-controlled exosuits have numerous sensors fitted into the build that capture nerve signals and control torque, pressure, tilt, and rotation.
- Buttons/control panels: Some exosuits contain pre-programmed modes, which are normally controlled by the user or by the physical therapist. Most control panels are located on the walking aids.
- Joystick: This is commonly found in active exosuits that provide all the energy required by the wearer.
- Mind-Controlled: These use an electrode skull cap as the main method of control.
No-control: Most passive exosuits do not have control buttons and respond to the mechanical movements of the wearer.
Types of Medical Exoskeletons

All exoskeletons are not built equally. They have different features and capabilities. In addition, the use of medical exoskeletons may differ between individuals based on the extent of injury and their recovery capacity. Exoskeletons are normally divided into:
- Upper Body Exoskeletons
Upper body exoskeletons are built to support the upper extremities, including the arms and torso. They are specifically designed to help patients with upper-body motor rehabilitation by positioning the shoulder, arm, and elbow through specific motions and orientations. They are extremely important to therapists because they can be used for intense motor exercises and task-specific movements.
- Lower Body Exoskeletons
Rehabilitative lower body exoskeletons are made for patients with lower limb motor dysfunctions to enable the recovery of lower extremity mobility. They normally use impedance control to generate resistance forces which are essential for rehabilitation training. Lower body exoskeletons have the ability to control joint movement in the hip, knee, and ankle.
Benefits of Using Exoskeletons After Spinal Cord Injuries

Exoskeletons are advantageous for patients and therapists alike. They have the ability to reduce the burden on therapists and help with quantitative data collection and patient evaluation.
- Gait Training:
Gait training consists of walking practice with the aim of helping the patient regain their normal walking gait. Using exoskeletons has the potential to make gait training easier and more convenient for therapists, given the numerous support features they offer. For instance, free-standing exoskeletons help patients to exercise in upright positions, which would be almost impossible and cumbersome without the use of exoskeletons. [8]
A 2008 gait training study carried out on two stroke survivors reports that “by the end of the training the gait pattern of the patients improved and became closer to a healthy subject’s gait pattern.” Improvement in this study was defined as “the increase in the size of the patients’ gait pattern, increased knee and ankle joint excursions and increase in their walking speeds on the treadmill.” [9] Exoskeletons also have unique features that help with rehabilitation. For example, the EksoNR has sensors that are made to monitor your patient’s leg movements and regulate their gait patterns. [10]
- Bladder and Bowel Function:
The use of exoskeletons may improve your patient’s bladder and bowel function. This is according to feedback that was received by researchers at the Spinal Cord Injury Model System Centers (SCIMS) from focus groups held with 30 therapists. They record that, “patients who gained the ability to stand and walk with an exoskeleton often developed better endurance, improved their bowel and bladder control, and were less likely to develop urinary tract infections.” [11]
Scientists believe that engaging patients in physical activities and maintaining upright postures may play a role in improving bowel motility. A 2019 study tested bowel management after exoskeleton training and reported an improvement of up to 80%. [12]
- Improved Muscle Strength and Spasticity:
Incorporating exoskeletons in your physiotherapy treatment may help patients improve their muscle strength. A 2021 study examining the effects of exoskeletons in physiotherapy observed that the use of exoskeletons improved grip strength, quadriceps strength, and lower limb motor function. [8] This was also observed in a 2019 study that reported exoskeletons improved muscle strength after a Manual Muscle Strength Test, “total score from both sides were: P3 UEMS increased from 30 to 37, and LEMS from 23 to 25; P11 UEMS increased from 33 to 37, and LEMS from 27 to 30, where the maximum score for UEMS and LEMS is 50.” [13]
Another study conducted on patients who had a stroke concluded that the use of exoskeletons in therapy improved the tibialis anterior muscle strength and lower limb motor function of the patients. [14]
- Improved Patient Moods:
Though not a significant benefit, the use of exoskeletons in therapy can help improve your patient’s moods. A 2021 study examining the effects of exoskeletons on patients with spinal cord injuries shows improved moods in one of the patients during the rehabilitation phase. It also reports a decrease in fatigue and an improved quality of life. [8] Since robotic exoskeletons are a “new” technology in rehabilitation, they can be exciting for patients and may motivate them to exercise more. Some therapists also report that exoskeletons offer extra psychological benefits to patients. For instance, patients reported psychological effects of having eye-to-eye conversations with others and also increased engagement in daily activities. [11]
- Patient Independence:
Exoskeletons can help patients gain some independence in their day-to-day activities like moving and walking around. Before the invention of medical exoskeletons, patients had to rely on their therapists to move around and exercise. However, that is no longer the case. They can now exercise and ambulate on their own, which gives them a sense of independence. Physical therapist Kyle McIntosh says, “The exoskeleton lets patients take actual steps, which is not only more realistic but much less cumbersome,” McIntosh also says, “Every step is different with this device, so patients learn from their mistakes in real time. Patients really like to use the device; it gives them hope.” [6]
Conclusion

Rehabilitative technology has come a long way, from crutches to walkers to wheelchairs and now, robotic exoskeletons. Robotic-assisted rehabilitation holds a lot of promise for both patients and physical therapists alike. Several studies have shown the potential benefits of exercising in a free-standing exoskeleton for patients with spinal cord injuries. If you are a physical therapist, this is the next medical technology shift that will help you offer next-level therapy solutions for your patients.
Ekso Bionics has been at the forefront of creating the best quality medical exoskeletons for more than a decade now. Our EksoNR was one of the first FDA-approved medical exoskeletons for rehabilitation, and it continues to be the exoskeleton of choice for many mobility rehabilitation clinics. Please review our indications for use to determine eligibility. [15]
References:
- Spinal cord injury https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury#:~:text=Key%20facts,traffic%20crashes%2C%20falls%20or%20violence. }
- Exoskeletal Assisted Rehabilitation After Spinal Cord Injury https://www.sciencedirect.com/topics/nursing-and-health-professions/exoskeleton-rehabilitation
- Spinal Cord Injury https://www.ninds.nih.gov/health-information/disorders/spinal-cord-injury
- Rehabilitation Therapies in Spinal Cord Injury Patients https://www.intechopen.com/chapters/72439
- Robotic Rehabilitation and Spinal Cord Injury: a Narrative Review https://pubmed.ncbi.nlm.nih.gov/29987763/
- Spinal cord injury patients may benefit from using exoskeleton earlier in treatment https://ucalgary.ca/news/spinal-cord-injury-patients-may-benefit-using-exoskeleton-earlier-treatment
- Types And Classifications of Exoskeletons https://exoskeletonreport.com/2015/08/types-and-classifications-of-exoskeletons/
- Physiotherapy using a free-standing robotic exoskeleton for patients with spinal cord injury: a feasibility study https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-021-00967-4
- Robot Assisted Gait Training With Active Leg Exoskeleton (ALEX) https://ieeexplore.ieee.org/document/4663875
- https://eksobionics.com/eksonr/
- Robotic Exoskeletons May Provide Health Benefits for People with Spinal Cord Injuriesnhttps://naric.com/?q=en/content/robotic-exoskeletons-may-provide-health-benefits-people-spinal-cord-injuries
- Changes in Bowel Function Following Exoskeletal-Assisted Walking in Persons with Spinal Cord Injury: An Observational Pilot Study https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7145720/
- Retraining walking over ground in a powered exoskeleton after spinal cord injury: a prospective cohort study to examine functional gains and neuroplasticity https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6868817/
- Impacts of a lower limb exoskeleton robot on the muscle strength of tibialis anterior muscle in stroke patients https://www.researchgate.net/publication/344023059_Impacts_of_a_lower_limb_exoskeleton_robot_on_the_muscle_strength_of_tibialis_anterior_muscle_in_stroke_patients/fulltext/5f519787a6fdcc9879c9cc2f/Impacts-of-a-lower-limb-exoskeleton-robot-on-the-muscle-strength-of-tibialis-anterior-muscle-in-stroke-patients.pdf
How Do Exoskeletons Prevent Work Injuries?
Work injuries are any injuries that arise during the course of employment. They may be categorized as traumatic, chronic exposure, psychological or emotional injuries. Among industrial workers, traumatic injuries are the highest due to the physically demanding nature of their jobs. This leads to Workplace Musculoskeletal Disorders (WMSDs) such as strains, sprains, bone fractures, back pain, carpal tunnel syndrome, tendonitis, osteoarthritis, hernia, among others.
Construction and industrial workers are at a higher risk of WMSDs, given the physical demands of their jobs. WMSDs are any conditions that involve soft tissues like muscles, nerves, cartilage, etc. According to the Centers for Disease Control and Prevention (CDC), construction workers have increased workplace musculoskeletal injuries associated with exposure to vibrations, awkward postures, and repetitive tasks during work. [1]
However, all is not lost. Ergonomic innovations and technologies like exoskeletons may hold the answer to reducing workplace-related injuries. They are task-specific robotic tools that help with reducing the load of repetitive work, reducing discomfort in awkward postures, and bearing extra weight on the body. Exoskeletons have wide applications and may be useful in a variety of industries such as, automotive, manufacturing, logistics, construction, and shipping industries.
Common Causes of Workplace Musculoskeletal Injuries
Construction environments are typically overflowing with activity and demand high amounts of physical exertion. This typically leads to overexertion as a result of lifting, carrying, pulling, holding, and pushing tasks – all inevitably leading to injury. In construction, workplace musculoskeletal injuries are commonly caused by repetitive work, strenuous work positions, continuous exertion and vibration.
- Repetitive Tasks
Repetition plays a big role in workplace injuries. Did you know workers lift their arms up to 4,600 times a day on average — consider how much toll this takes on their upper extremities. Repetitive tasks are very hazardous because they lead to repeated strain in the same muscle groups and joints. This can lead to injury and disability, which eventually impacts productivity and work efficiency. If the cycle time of your job is 30 seconds or less, it is classified as a repetitive job and may expose you to a higher risk of work injury.
- Awkward Work Positions
Awkward positions include any position that differs from the natural body positions we should inhabit while working. Even maintaining the same position in normal postures for long periods of time usually leads to fatigue. Now consider unnatural work positions; they lead to muscle inefficiency and exertion, which inadvertently leads to musculoskeletal injuries. Examples of common awkward postures include prolonged standing, which may cause fatigue and lower back pain, bending forward, which can cause lower back injuries, and reaching overhead which may cause damage to your shoulders and arms. Sometimes, maintaining fixed positions may also lead to stiffness and injury.
- Continuous Exertion
The human body is not designed to take on continuous force and exertion. It needs recovery time in order to regain strength and vitality. Unfortunately, long work hours subject our bodies to constant exertion with limited recovery time. This leads to accumulated fatigue in certain body parts like the lower back, which makes them prone to injury. Continuous exertion exposes the same muscle groups and body parts to wear and tear, which may lead to injury if not attended to.
According to the Center for Construction Research and Training, overexertion is the leading cause of WMSDs, causing up to 67% of musculoskeletal disorders among construction workers in 2015. [2] Apart from causing WMSDs, overexertion also results in lost productivity, disability, and costly medical expenses. The effects of overexertion are also experienced on a more significant economic scale. According to the CDC, “the economic burden of construction industry worker’s compensation costs brought on by WMSDs in the United States has been estimated to be more than $2 billion annually (Liberty Mutual 2021).” [1]
- Vibration
Vibration may affect the whole body or a specific body part. It usually affects workers who operate power tools, machines, and even trucks. Vibration can affect the nerves, muscles, tendons, and joints, and it usually results in fatigue, pain, loss of touch, and numbness. Continuous exposure to vibration is very detrimental to workers.
What Are Exoskeletons?

Exoskeletons, also known as exosuits, were first developed in 1890. They are wearable frames that provide support and enhance the wearer’s capabilities. Exoskeletons amplify the strength of the wearer and augment their physical performance. While they do not give superhuman strength to the individual, exoskeletons are instrumental in increasing productivity, supporting heavy lifting, and reducing physical workload. This has an overall positive effect on reducing musculoskeletal injuries.
Exoskeletons can be classified into two: passive or active. Passive exoskeletons are mechanical, use springs, and counterbalance forces to operate, whereas active exoskeletons use powered mechanisms like hydraulics and electric motors. Despite their differences, passive and active exoskeletons are equally used in providing support to the waist, shoulder, and thigh. However, research shows passive exoskeletons are preferred in industrial workplaces. [3]
Types of Industrial Exoskeletons

There are two main types of industrial exoskeletons: upper-body exoskeletons and lower-limb exoskeletons. Although both reduce the risk of WMSDs, they operate differently and provide support to different parts of the body.
- Upper-Body Exoskeletons
Upper-body exoskeletons are designed similarly to a backpack. They support the upper extremities and play a significant role in reducing shoulder injuries, particularly among workers who engage in repetitive overhead work. The exoskeleton engages every time you raise your arms or lift something and creates a counterbalancing force that reduces the total load and provides support. This makes completing the task at hand easier and safer.
Upper-body exoskeleton technology is continuously improving and evolving. For instance, Ekso Bionics changed the Ekso EVO from a “backpack” design to a “strap” design that makes the exoskeleton extremely lightweight and comfortable to wear. [4] EVO provides 5 – 15 lb. (2.2 – 6.8 kg) of list assistance per arm to give your natural strength a boost throughout your work day. This is not intended to give you super strength but instead give you super endurance and reduce fatigue so that you have more energy and less soreness at the end of your shift. Whatever payload you normally lift (a 4 lb. torque wrench, a 10 lb. component, or even just the weight of your arm) will feel lighter with the boost you get from your EVO.
- Lower-Limb Exoskeletons
Lower-limb exoskeletons are generally designed to support the lower body and augment strength when moving or performing heavy tasks. They are made to support joints like your hips, knees, and ankles. Lower-limb exosuits offer support any time you bend or lift a heavy load by passing on the weight to your legs, thus relieving the lower back from heavy weight. [5] Lower-body exoskeletons normally follow the wearer’s motions and respond to the different actions they take.
Benefits of Using Exoskeletons at Work

Exoskeletons present many benefits to construction workers. They provide ergonomic assistance when performing repetitive tasks, enhance worker safety when working in hazardous environments and even reduce fatigue. They remain to be an unrivaled innovation for reducing Workplace Musculoskeletal Disorders and present a practical solution to workplace safety.
- Improved Comfort At Work
Exoskeletons are lightweight, easy to use, and are made with comfortable materials that help reduce discomfort when wearing them. For instance, Ekso EVO is made with a compact design that is designed to minimize the exoskeleton’s weight for easy wearability. Ekso EVO also has minimal touch-points, which help you keep cool while working, improving your overall comfort.
- Reduced Fatigue
Exoskeletons reduce fatigue by bearing the weight of heavy loads. They do this by distributing the wearer’s weight evenly to the core and waist, thus reducing repetitive force on specific body parts. Some exoskeletons also use counterbalance forces to provide support to the wearer. According to the CDC, “Back assist exoskeletons were found to reduce back muscle activity by 10-44% during handling tasks, and hip extensor muscle activity was reduced by 24% in laboratory studies.” [1] In a 2015 study, researchers reported up to 80% muscle activity reductions due to the use of active exoskeletons. [6]
- Increased Productivity
Exoskeletons are great at boosting productivity and efficiency. They help workers lift heavier loads for more extended periods of time, effectively increasing the amount of work one can do per day without compromising physical health. Exoskeletons also improve speed and accuracy, which results in a more efficient workflow. Apart from productivity, exoskeletons help workers end shifts with more energy and less soreness, which goes a long way in improving morale. Increased productivity also positively affects a company’s bottom line due to improved output and less sick days.
- Reduced Injury and Sick Days
According to the U.S. Bureau of Labor Statistics, workplace injuries result in an average of 34 days of sick leave. [7] According to the 2021 AmTrust Contractor Risk Report, 34% of workplace injury claims come from plumbers and 27% from electricians who have repetitive overhead tasks, which lead to strain and musculoskeletal injuries. [8] Exoskeletons can help reduce workplace injuries which effectively reduces the number of sick days workers have to take.
Exoskeletons reduce the load that workers bear and offer support to the shoulder and arms in case of overhead tasks. This helps minimize repetitive wear and tear on body parts, reducing the number of work-related injuries. Ford Motor Company has been at the forefront of acquiring exoskeletons for their workforce, and since 2011, they have recorded an 83% reduction in workplace injuries in departments that use exoskeletons. [9] The CDC also believes that exoskeletons are the best alternative to reducing musculoskeletal injuries and associated costs in different industries. [1]
- Improved Work Quality
Exoskeletons may help improve the quality of work since workers are less fatigued, which contributes to alertness and accuracy. This results in a higher level of work output within shorter periods of time, boosting productivity. [10]
Conclusion

Occupational exoskeleton technology is undeniably the next-best solution to reducing workplace injuries, especially in industries that require heavy lifting and expose workers to repetitive tasks and awkward working positions. Exoskeletons are beneficial in reducing strain, fatigue, injury, and improving overall productivity. Just to show how critical exoskeletons are for work, in 2019, Toyota made upper-body exoskeletons a mandatory part of Personal Protective Equipment (PPE) for workers who engage in overhead work.
Ekso Bionics has been at the forefront of producing the best-in-class wearable technology for years, and all our exoskeletons are made with insight from industry experts and stakeholders. Our Ekso EVO exoskeleton vest is the product of choice among workers who care about their health and comfort while performing their daily activities. Ekso EVO remains to be the go-to exosuit for our partners, Boeing and Ford. [4]
References:
- Exoskeletons: Potential for Preventing Work-related Musculoskeletal Injuries and Disorders in Construction Workplaces https://blogs.cdc.gov/niosh-science-blog/2022/02/03/exoskeletons-construction/
- Chart Book (6th edition): Fatal and Nonfatal Injuries – Musculoskeletal Disorders in Construction and Other Industries https://www.cpwr.com/research/data-center/the-construction-chart-book/chart-book-6th-edition-fatal-and-nonfatal-injuries-musculoskeletal-disorders-in-construction-and-other-industries/
- The Effects of Upper-Body Exoskeletons on Human Metabolic Cost and Thermal Response during Work Tasks—A Systematic Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7600262/
- https://eksobionics.com/ekso-evo/
- Exoskeletons are reducing ergonomic injuries https://www.thesafetymag.com/ca/topics/technology/exoskeletons-are-reducing-ergonomic-injuries/184498#:~:text=%E2%80%9CWe%20know%20that%20in%20a,compressive%20forces%20in%20the%20spine
- Exoskeletons for industrial application and their potential effects on physical work load https://pubmed.ncbi.nlm.nih.gov/26444053/
- Occupational Injury and Illness Classification Manual https://www.bls.gov/iif/oshoiics.htm
- AmTrust 2021Contractor Risk Report https://amtrustfinancial.com/contractor-report
- How Exoskeletons Impact The Workplace https://eksobionics.com/how-exoskeletons-impact-the-workplace/
- https://eksobionics.com/manufacturing/
How Exoskeletons Are Beneficial for Acquired Brain Injuries
Acquired brain injuries (ABI) are more common than we’d like to imagine. According to the Brain Injury Association of America (1), brain injury is a leading cause of death and disability in the U.S., with at least 2.8 million Americans sustaining a traumatic brain injury each year. In the U.K. (2), approximately 348,453 ABI patients were admitted to the hospital in 2017, which translates to one person every 90 seconds. These statistics are not limited to the U.S. and U.K.; a similar pattern is observable in other parts of the world. Despite the bleak outlook from these statistics, modern medical exoskeletons offer hope and an opportunity for recovery from brain injury patients who’ve lost their mobility.
This article investigates the causes, types, and effects of brain injuries. It also looks into the various treatments available with a special focus on medical exoskeletons and how they are improving mobility rehabilitation in ABI patients.
What Is An Acquired Brain Injury?

The Brain Injury Association of America describes an acquired brain injury (ABI) (3) as any injury to the brain that occurs after birth and affects the brain’s physical integrity, functionality, and metabolic activity. In other words, the term ABI is used as an umbrella term for all brain injuries. An acquired brain injury can occur in many different ways. It can be sudden, resulting from a blow to the head, stroke, infection, trauma, or lack of oxygen. It can also result from a long-term process such as degenerative disease, prolonged drug abuse, or a growing tumor. An ABI may lead to cognitive, sensory, physical, and behavioral changes like physical weakness, impaired vision, forgetfulness, mood swings, slurred speech, and impaired mobility.
Major causes of ABI include:
- Substance abuse – Psychoactive drugs (stimulants, depressants, and hallucinogens) can poison the brain, leading to impairment.
- Age-related and degenerative conditions – As we get older, we become more susceptible to degenerative brain conditions like Dementia and Parkinson’s disease, which increase the risk of developing a brain injury.
- Diseases – Such as meningitis, Alzheimer’s disease, brain abscess, multiple sclerosis, and cancer.
- Anoxia and Hypoxia – This is the lack of sufficient oxygen supply to the brain. It can result from strangulation, heart attack, or near-drowning.
- Concussion – This is caused by a blow to the head. It can occur in vehicle or sporting accidents, fights, or falls. It is the most common type of brain injury.
- Stroke – which happens when there is an interruption of blood supply to the brain. It can be caused by blocked or broken arteries, which in turn leads to damaged brain tissue.
Types and Effects of Acquired Brain Injuries
There are two types of acquired brain injuries: traumatic brain injury (TBI) and non-traumatic brain injury. A traumatic brain injury is any type of brain injury that is caused by an external force—for example, a blow to the head, car accident, or a fall. However, not all head injuries cause a TBI because you can sustain an external impact to the head that doesn’t alter the brain in any way. On the other hand, a non-traumatic brain injury is caused by internal factors like oxygen deprivation, tumors, substance abuse, and strokes. Non-traumatic brain injuries can be sudden, as in the case of a stroke, or can progress over time, as in the case of a degenerative brain disease.
Acquired brain injuries affect people differently based on the extent of damage sustained to the brain and the areas affected. For instance, one type of injury may affect a person’s mobility, while another may affect their speech or cognitive functions.
Here’s a detailed list of the effects of acquired brain damage (4):

Acquired Brain Injury Therapy

A wide range of treatments are available for people with an acquired brain injury ranging from surgery to speech therapy to cognitive therapy and physical therapy. Each treatment is dependent on the effects the patient is experiencing. Generally, all types of treatment are designed to help improve and recover affected functionalities, but recovery differs from person to person. It usually depends on the extent of brain damage, the general health of an individual, and the quality of treatment.
- Physical therapy: The main function of physical therapy is rebuilding mobility after sustaining an ABI. It focuses on areas like muscular strength, balance, coordination, and flexibility. It is normally conducted by a physiotherapist who is trained in physical mobility restoration. Physical therapy can also be aided by the use of a medical exoskeleton.
- Occupational therapy: Occupational therapy typically goes hand in hand with physical therapy. Occupational therapy is aimed at helping you relearn daily living activities like bathing, making your bed, dressing, etc. It is conducted by occupational therapists who are experts in training people how to regain independent functioning in daily activities.
- Cognitive-behavioral therapy (CBT): This addresses the cognitive and behavioral functions that might have been affected after sustaining an ABI. It is common for patients to experience stress, anxiety, depression, and panic attacks during recovery. CBT therapy helps them learn how to manage their emotions by teaching how to identify unhealthy thinking patterns and healthy emotion management techniques.
- Speech therapy: Speech therapy is a recommended treatment option for people with speech impediments like communication disorders and apraxia. Speech pathologists help patients regain their communication and language skills by taking them through speech recovery exercises.
Exoskeleton Benefits for Acquired Brain Injuries

Medical exoskeletons have gained a lot of popularity in the medical field and are a great physical therapy treatment option. Instances of health-related applications (5) for exoskeletons include stroke, spinal cord injury, acquired and traumatic brain injury. They offer benefits like improved step quality, muscle strength, and postural balance, as discussed below.
- Improves Patients’ Orientation to Midline
The midline is an imaginary line that runs from the top of your head to the point between your feet. Proper midline orientation (6) means that your brain’s left and right hemispheres are working together and not in isolation. This helps with balance perception when walking and conducting other activities. However, some patients, who have sustained an ABI, may lack proper orientation due to their injury, which leads to reduced limb and motor control, and postural misalignment. Exoskeletons help match both sides of the body through kinesthetic and proprioceptive systems, leading to an improved orientation to the midline.
- Allows For Easier Weight Shifting
Proper weight shifting allows body weight to be evenly distributed on all limbs. However, this may be impossible for people diagnosed with an ABI. (7) This is where exoskeletons come in handy. Medical Exoskeletons offer posture and limb support (8) which helps patients bear their own weight properly for proper postural alignment and blood circulation within the limbs.
- Improves Stepping Quality
According to a 2020 study, (9) conducted on adolescents and young adults with acquired brain injury, gait training with exoskeletons is an effective physiotherapy treatment option that leads to improved motor function in patients. Many patients struggle with ambulation (movement), but with the help of medical exoskeletons, they can increase their neurological recovery through movement. Dr. Karunakaran reported, “At the end of the 4-week training, participants had progressed to a more normal gait pattern, including improved loading, a longer step length, and faster walking speed.” (9)
- Increases Lower Extremity Muscle Strength
Exoskeletons amplify human strength and endurance during movement, improving muscle strength. One 2020 study (10) on the impact of a lower limb exoskeleton robot on muscle strength showed that patients with stroke hemiplegia, who trained using lower limb exoskeletons, experienced an increase in the tibialis’ anterior muscle strength compared to those who relied on conventional rehabilitation.
- Great for Repetitive Motions
Repetition in motor rehabilitation is a crucial element of recovery, and exoskeletons provide patients with high repetitions of complex gait cycles. Additionally, where a patient used to only take few steps a day with the help of a physical therapist, they can take more steps with the help of a medical exoskeleton. (8)
- Provides Support to Physical Therapists
Physical therapists can only do so much. They are human and prone to fatigue and exhaustion. A 2020 study (11) revealed that stroke patients get an average of 14 minutes of physiotherapy per day, which is less than the recommended threshold. However, exoskeletons have unlimited capacity, and using them reduces the workload for physical therapists and increases the quality of rehabilitation for patients. Exoskeletons allow for increased intensity, longer duration of practice, and increased patient engagement. (12) They also provide a chance for physical therapists to challenge their patients since they require active participation, which is known to improve brain plasticity. (13)
Diane Patzer, a physical therapist from the Rehabilitation Institute of Michigan (8), says, “We went from taking 20 steps with three physical therapists to taking hundreds of steps in a session with one.”
Conclusion
Medical exoskeletons are a great mobility recovery tool to use in physical therapy. They enhance motor rehabilitation by giving patients the confidence to get up and begin walking. They eliminate a patient’s fear of falling, which helps them start their mobility recovery faster. And above all, exoskeletons are very engaging compared to other tools. This makes them a great tool for patients who want to increase their chance of mobility recovery.
Ekso Bionics has been at the center of developing medical exoskeletons for more than a decade. Our products are created by clinical and engineering experts in conjunction with feedback from industry leaders. EksoNR, a product of Ekso Bionics, is the first and only FDA-cleared medical exoskeleton for rehabilitation use with ABI. EksoNR is versatile and can be used by ABI patients at any stage in their recovery journey.
References:
(1) https://www.biausa.org/public-affairs/public-awareness/brain-injury-awareness
(2) https://www.headway.org.uk/about-brain-injury/further-information/statistics/
(3) https://www.biausa.org/brain-injury/about-brain-injury/basics/overview
(4) https://www.headway.org.uk/about-brain-injury/individuals/effects-of-brain-injury/
(5) https://eksobionics.com/indications-for-use/
(6) https://eksobionics.com/acquired-brain-injury/
(7) The scaling of postural adjustments during bimanual load-lifting in traumatic brain-injured adults
(8) https://eksobionics.com/eksonr/
(9) Kinetic Gait Changes after Robotic Exoskeleton Training in Adolescents and Young Adults with Acquired Brain Injury
(10) Impacts of a lower limb exoskeleton robot on the muscle strength of tibialis anterior muscle in stroke patients
(11) Factors influencing the amount of therapy received during inpatient stroke care: an analysis of data from the UK Sentinel Stroke National Audit Programme
(12) Exoskeleton Training May Improve Level of Physical Activity After Spinal Cord Injury: A Case Series
(13) Effects of Physical Exercise on Neuroplasticity and Brain Function: A Systematic Review in Human and Animal Studies
Patient Success Story: Megan
A patient story we would like to share with you features one of our Patient Ambassadors, Megan Burns, from Greater Chicago.
Before her injury, Megan was a healthy active adult in her early thirties. Megan enjoyed playing tennis a few times a week at her neighborhood courts in the summer. On Sundays, Megan would play golf with her partner Brian and her Aunt and Uncle. She also went on daily walks with her dog Chip. Megan and Brian also enjoyed hiking in Lake Geneva on the scenic lake path in the spring, summer, and fall in Wisconsin.
Megan also liked a little adventure. Shortly before her injury she hiked up the Devils Doorway at Devil’s Lake in Wisconsin, enjoyed zip lining down mountains in the Jamaican rainforest, and walked up the 600-foot-long landmark Dunn’s River waterfall. Every May, Megan and her cousin Mindy would go for an adrenaline rush and ride all the big roller coasters at Six Flags Great America; rain or shine!
Megan’s entire life changed in December of 2015 when she had a stroke in her spinal cord caused by a ruptured arteriovenous malformation (AVM). A spinal AVM is a rare, abnormal tangle of blood vessels on, in, or near the spinal cord. Due to the spinal cord stroke, Megan underwent a resectioning of her spinal cord which was performed in February of 2016. After her AVM and resectioning surgery, Megan was diagnosed with a T-12- incomplete spinal cord injury (iSCI).

Post-injury, Megan used a wheelchair to get around. Over time with physical therapy and lots of hard work, she was able to progress to walking with a wheeled walker and eventually a straight cane and AFO (ankle foot orthoses) braces. Doctors were thrilled with this progress since her original prognosis was that she would always need to use a wheelchair. Although the progress was great, Megan did not accept that she had reached the end of her journey towards walking independently. She would rely on her cane for stability and drag her legs through the motions of walking. For Megan, this was not the best solution and was not the peak of her progress!
Megan was introduced to Ekso in the fall of 2017 which was two years after her injury. Still not satisfied with the quality of her gait, she went to the Shirley Ryan AbilityLab website to look for rehabilitation help. Megan saw they were seeking participants for a study called WISE (Walking Improvement for SCI with Exoskeleton) which was looking at comparing Ekso rehab with traditional rehab for incomplete spinal cord injured patients. She fit the study criteria and signed up immediately. Luckily, Megan started as a participant of the trial in the first quarter of 2018. She would end up using Ekso three days per week for twelve weeks and here is what happened next:
First session – Megan found her balance with the help of the preGait functions and her posture began to recover.
Third session – She became very comfortable and confident in the device. Megan learned how to work together with the exoskeleton, that Ekso was not walking for her, and stopped fighting it. At this point she really started to learn from it.
“It was here that I realized I need to take the information I learned in Ekso and carry it over into real life. This is where I realized the importance of Ekso and the steps. I was taking 500+ steps in my first few sessions of 45 minutes each. That was more steps than I was taking in days. Not only was I thrilled at the step quantity, but also the quality. The step pattern in Ekso is natural and would not allow me to drag my toes. You can only take quality steps in the device.”
Fifth session – Together with her therapist, Megan realized she had not used her calves in two years. She finally started pushing with her calves again to clear the toes that were curled under from foot drop. Even today, Megan says, “I still hear my PT when I am walking to PUSH.”
Session twelve – Megan stopped using her AFO because she was engaging her calves with every step. By the twelfth session she was taking 900+ steps in Ekso each time, including backward and forward walking.
By session twenty Megan was walking in the community completely unassisted—no more cane!
And the best news of all, by the thirty-sixth session in Ekso Megan was back to golfing, a goal of hers since her injury back in late 2015.
“Now, in outpatient, my therapists are kind and patient, but also challenge me. MidAmerica Rehabilitation Hospital is now my family.”
Today, Megan still can’t feel her legs from the waist down but has been able to build up her muscles in her legs in order to keep walking. She has carried on with all the lessons from her Ekso training and has been walking unassisted for nearly two years! She has returned to using Ekso in the outpatient setting, for what she calls “tune ups”. As a busy professional and someone who travels for pleasure as often as she can, Megan tends to get busy with life moving quickly and returns to some old habits—short steps, not weight-shifting, and dragging her toes.
“Every time I use Ekso I learn something new and take it with me. I do have to think of every step I am going to take, but now it is so much easier.”
Megan would like to stress how much she believes in Ekso. So much so, that she would drive more than two hours round-trip for the twelve-week duration of the study to get into the device to keep learning to walk. We are so thrilled with Megan’s progress and her incredible return to the full life she was enjoying prior to her injury. Since regaining her balance and strength she has been able to get back to her adventurous side and has been parasailing, scuba diving, cliff jumping, and hiking at the Grand Canyon. She also has returned to joining friends for concerts and still makes her annual trip to Six Flags to ride the roller coasters with her cousin.
Megan’s success with Ekso has also led to her joining Ekso Bionics as a Patient Ambassador so she can continue to share her story with as many people as possible and spread hope.

5 Amazing Ways to Use Exoskeletons for Construction
Whether you are lifting heavy objects or completing light and repetitive tasks, construction exoskeletons are your best chance of injury prevention and productivity enhancement. In 2017 alone, there were at least 12,000 injuries per month in the construction industry (1), many of which could have been prevented with the use of exoskeletons. According to research (2), exoskeletons reduce human metabolic cost and thermophysiological response during upper-body work tasks, which translates to less fatigue and strain for workers., resulting in increased productivity. For construction and warehouse workers, exoskeletons are the next industrial shift that will lead to increased efficiency and productivity.
In this article, you will learn what exoskeletons are, how they are applied in construction, and their benefits. Let’s dive in.
What Are Exoskeletons?
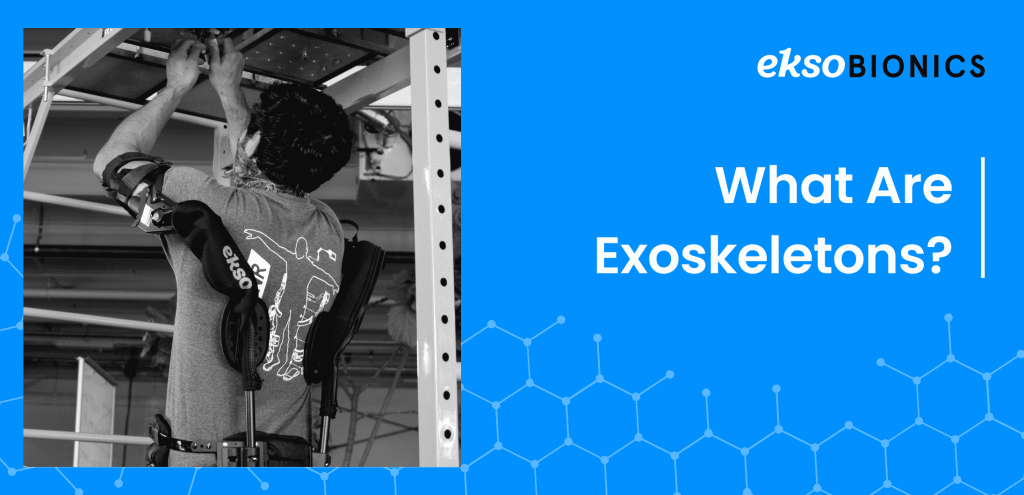
Exoskeletons, also referred to as exosuits, powered-armor, or exo frames, are wearable external frames that offer extra support and enhance a person’s biomechanical capabilities. Think Iron Man from the Avengers, but in real life. The exoskeleton acts as a strength amplifier that augments physical performance or a corrective device for restoring mobility.
Some people believe that exoskeletons are a new “thing”. However, this technology has been in existence since 1890 but has only gained more traction in recent years due to accelerated technology developments. The early model, designed and patented by Nicholas Yagn (3), was a spring-operated device that enhanced the user’s ability to run and jump.
Today, exoskeletons have wide applications and are used in the military, medical, and construction fields. In the medical industry, physical therapists use them as locomotive assistance and gait training devices for patients who have a condition or injury that affects mobility. While in the construction industry, they are primarily used to help workers with their upper extremity mobility by reducing strain and increasing productivity.
There are two types of exoskeletons, powered and passive. A powered exoskeleton contains electric motors, levers, hydraulics, and other technologies that enable limb mobility with increased endurance and strength. It works by sensing the wearer’s motions, sending signals to the motors, and offering the necessary support. A passive exoskeleton differs from a powered exoskeleton because it is purely mechanical. However, they both offer benefits such as shoulder, waist, or thigh support. Additionally, it offers movement assistance when lifting heavy items. Powered exoskeletons are mostly used in military and physical therapy, while passive exoskeletons are more commonly used in construction and other industrial industries.
Exoskeletons and Injury in the Construction Industry

Did you know that the rate of work-related musculoskeletal disorders in construction is 16% higher than in all industries combined?(4) This statistic alone should be enough to point you to the most significant challenge that construction workers face: workplace injury. According to the Construction Chartbook (5), the most common injuries in construction are located in the back, shoulders, and other joints. This can be attributed to the long and repetitive tasks that eventually lead to overexertion and strain to workers’ bodies.
“The most common cause of workplace injuries was overexertion and fatigue. With 20% of construction workers reporting severe pain, construction workers are five times more likely to report poor health. US companies pay nearly $62 billion per year for workplace injuries.” (6)
Workplace injury results in lower productivity, which accumulates to more than 104 million lost production days.(1) In addition, it impacts construction workers’ morale as the uninjured employees have to take up bigger workloads to make up for the injured and recuperating workers. It also affects the injured person’s ability to complete future tasks and lowers their working lifespan.. However, organizations can avoid this by investing in construction exoskeletons.
In a study conducted in 2015 on the application of exoskeletons in industrial applications and their potential effects on physical workload, researchers discovered that exoskeletons greatly reduce fatigue while improving endurance (7). Additionally, exoskeletons reduce shoulder discomfort, thereby improving work quality and productivity among workers. Apart from decreasing the risk of workplace injury, exoskeletons also assist aging workers, and give them an opportunity to work beyond their age and physical limit.
Construction exoskeletons are the future of the construction industry due to the efficiency and productivity opportunities they present. Their primary purpose being: to improve the quality of life for construction workers and prevent injury.
You can use exoskeletons on the manufacturing floor to engage in long-intensive overhead work like installing sensors and filters without straining or injuring yourself. Benefits include joint support that’ll boost your endurance, productivity and prevent injury.
The Construction Exoskeleton Vest

Construction exoskeletons come in different shapes and variations suited to a specific task. Depending on the workload, it can be a full suit, a simple vest to support upper limb mobility or just a glove. Let’s take a look into an exoskeleton vest.
The construction exoskeleton vest is an upper-body exosuit specifically designed to support upper extremity mobility. Its main goal is to reduce workplace injury and worker fatigue by supporting muscle activity and joint movement. It also reduces discomfort when performing repetitive overhead tasks. Let’s establish one important fact; a construction exoskeleton won’t give you ‘Iron Man-level’ superhuman strength. In essence, the vest serves to reduce musculoskeletal loads. You’ll still lift an equal amount of load as you could before. The only difference will be that the load will be lighter and easier to carry since you’ll have additional muscle support.
The construction exoskeleton vest contains features like:
- Lightweight frame: This makes it easy and comfortable to wear.
- Durable materials: The vest is built for the construction environment where they can be exposed to the harshest element and function fully without breakage.
- Assistive: The Exo suit has an adjustable force assistance level that allows you to determine the amount of arm support you want from the suit.
- Natural-tracking: You can wear the suit and move naturally using your intuition, instincts, and reflexes to control it.
- Minimal contact points: This allows workers to work unhindered with a full range of motion and great airflow for comfort.
How Does The Construction Exoskeleton Vest Work?

Exosuits work in different ways depending on how they are powered. Mechanical exoskeletons, which do not use electricity, take weight from certain parts of the body and redistribute it to other areas. For instance, it can take weight from the arms or back when doing tedious overhead work and transfer it to your core to reduce fatigue and strain on muscles and joints. Mechanical exoskeletons are more advantageous since they don’t need to be recharged to use them. So, there’s no downtime. Additionally, they offer more longevity.
On the other hand, electric exoskeletons are more powerful and can handle more weight. They work by increasing pressure and strength in targeted areas as required. The frame responds to the wearer’s motion and provides support when needed. Due to their reliance on power, they can stop work if they run out of charge. In addition, you have to recharge them between uses.
The construction exoskeleton vest is one of the must-have technologies for construction, logistics, and warehouse workers, and for manufacturers who are interested in increasing occupational safety. It is the best solution to reducing muscle pulls, elbow and spinal injuries, and back sprains. It represents the coming together of man and machine to make work easier and more efficient. Let’s dive into the benefits more extensively below.
Fun Fact: The Master Mystery, released in 1919, is the first movie to feature a powered exoskeleton
5 Benefits Of Construction Exoskeletons
You can enjoy many benefits from using industrial exoskeletons, like lifting heavy loads, performing repetitive tasks, reducing the risk of injuries, supporting joints, and increasing work efficiency.
- Injury and Strain Prevention
Exoskeletons cut down on overexertion by supporting workers’ upper limbs when performing monotonous activities. They distribute the user’s weight evenly to the core and waist by reducing strain on the arms and shoulders. This leads to decreased workplace injuries like back sprains and shoulder injuries.
- Withstanding Repetitive Tasks
Picture a construction worker who has to raise their arms over their heads for hours on end plastering a wall or installing drywall. That’s a daunting task, but with a construction exoskeleton, their workload is made more bearable because they have extra support for their arms. They no longer have to go home with joint and back pains, and they can work for more hours without overexerting themselves and thereby increasing their productivity.
- Increased Productivity
Exoskeletons have been proven to increase workers’ endurance by reducing the amount of energy exerted on repetitive tasks. Additionally, since the frame takes on a portion of the musculoskeletal load, it reduces strain on the worker’s muscles and lowers fatigue. Coupled with less injury and strain, this becomes a great productivity enhancer for workers since they can work longer and more efficiently.
- More Work Accuracy
After endless hours of overhead work, accuracy is lowered due to muscle fatigue and exhaustion. However, with an exosuit, you can practically maintain most of your attention and focus on the task at hand without the distraction of strain and fatigue.
- More Opportunities For Aged Contractors
Due to the labor-intensive nature of construction work, older contractors are more likely to be limited by their physical abilities. But with a construction exoskeleton, these workers are able to handle more strenuous work effectively.
Conclusion

In recent years, the construction industry has experienced a lot of automation. However, not every task can be automated and replaced with a robot. There are specific, heavy and repetitive tasks that only humans can do. And the best option for attaining more efficiency and productivity in these non-autonomous tasks is to invest in well-produced exoskeletons. They are an innovative injury prevention solution and present great productivity potential in the construction industry.
If you are considering getting a construction exoskeleton, Ekso Bionics is your best choice. We are the leading company in exoskeleton technologies and have produced some of the best products in the world for the last 17 years. We’ve worked with the United States military, DARPA, Johns Hopkins, Shirley Ryan AbilityLab, Kessler Institute, the Department for Veterans Affairs, and UCLA, among others. Our products are FDA-Approved and are based on clinical experts and feedback from industry leaders.
References:
- https://eksobionics.com/eksoworks/
- The Effects of Upper-Body Exoskeletons on Human Metabolic Cost and Thermal Response during Work Tasks—A Systematic Review https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7600262/
- APPARATUS FOR FACILITATING WALKING, RUNNING, AND JUMPING. No. 420,179 https://patents.google.com/patent/US420179A/en
- Exoskeletons in Construction: Will they reduce or create hazards? https://blogs.cdc.gov/niosh-science-blog/2017/06/15/exoskeletons-in-construction/
- CPWR. The Construction Chartbook. Fifth Ed. CPWR- the Center for Construction Research and Training. Silver Spring, MD. April 2013. http://www.cpwr.com/publications/construction-chart-book
- https://eksobionics.com/construction/
- Exoskeletons for industrial application and their potential effects on physical work load https://pubmed.ncbi.nlm.nih.gov/26444053/